Adult Congenital Heart Disease
Applying Multimodality Imaging for Tricuspid Regurgitation
Three-dimensional echocardiography, cardiac CT, and MRI are becoming increasingly important in determining management strategies for tricuspid regurgitation. Weill Cornell faculty recently explored the role that multimodality imaging plays in the evaluation and treatment of this significant cardiovascular problem, which continues to be undertreated. Their review, published in the August 9, 2018 issue of Current Treatment Options in Cardiovascular Medicine, suggests that 2D and 3D transesophageal echocardiography for reconstruction are becoming increasingly important tools for surgical and transcatheter interventions. The technology offers continuous imaging to help confirm catheter and wire position and minimize fluoroscopy radiation. CT is important to preprocedure planning for transcatheter tricuspid valve therapy, while the main role of cardiac MR is in preoperative assessment.

Cardiac MRI shows Ebstein’s anomaly with apical displacement of the septal leaflet resulting in severe tricuspid regurgitation.
With new transcatheter options for managing tricuspid regurgitation emerging over the last few years, especially in higher risk patients, multimodality imaging is becoming integral to preprocedural, intraprocedural, and postprocedural intervention.
Treating Persistent Arrhythmias
While catheter ablation is commonly performed to treat atrial arrhythmias in ACHD, factors for predicting recurrence have not been adequately defined. A retrospective study conducted by Columbia researchers looked at catheter ablations for atrial arrhythmias performed in 125 patients with ACHD at NewYork-Presbyterian/Columbia over a 10-year period between January 2005 and February 2015.
Their analysis, published in the November 19, 2018 online issue of Congenital Heart Disease, revealed that body mass index and Fontan status were the only variables associated with recurrence, with BMI indicating a more significant risk independent of Fontan status. These findings may help guide treatment decisions for persistent arrhythmias.
Managing the Arterial Switch Patient
In the June 26, 2018, issue of Current Cardiology Reports, Weill Cornell faculty discuss the long-term management of patients with dextro-transposition of the great arteries (D-TGA). For the past three decades the standard of care to treat patients with D-TGA has been an arterial switch repair, which offers very successful outcomes. Branch pulmonary stenosis, coronary artery stenosis, and neo-aortic regurgitation are the most common complications, and careful evaluation of new symptoms or declining function is essential to prevent these long-term sequelae. Long-term management by adult congenital heart disease specialists, with the use of chocardiography and CT or MRI, is recommended for all patients with D-TGA.
Adult Congenital Heart Disease Procedures
Volume Based on Primary Procedure
2017
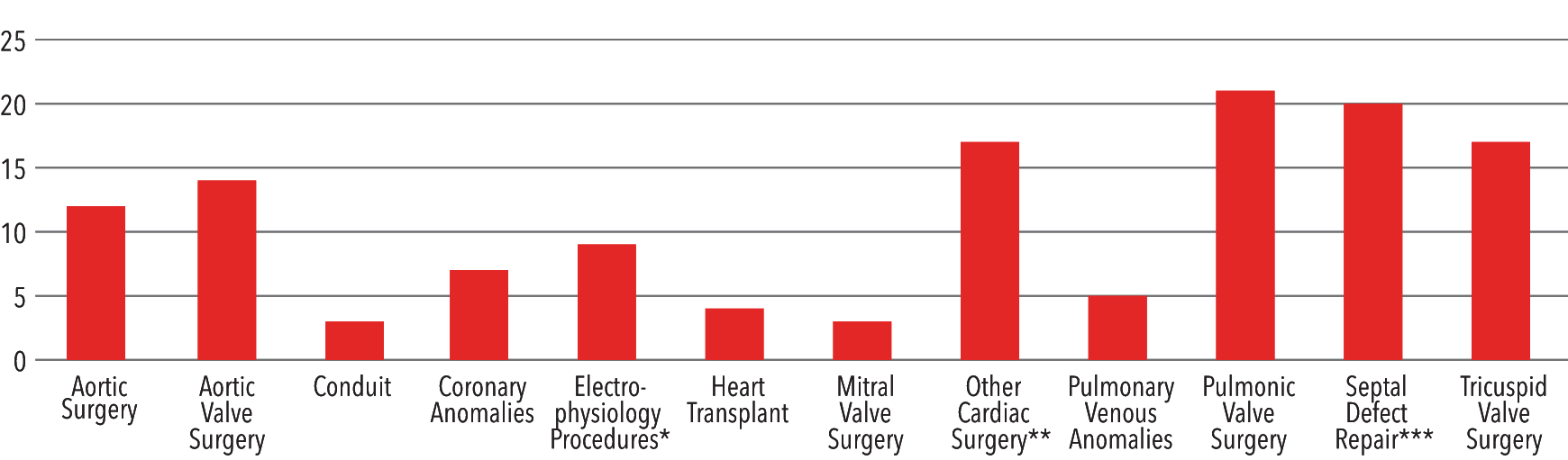
* Electrophysiological procedures included Maze, PMI; **Other cardiac surgery included ECMO, tetralogy of Fallot, mediastinal procedure, cone procedure, cardiac procedures, mediastinal procedure, miscellaneous procedures, removal of transcatheter delivered device from blood vessel, pulmonary artery reconstruction, left thoracotomy; ***Septal defect included ASD, AVSD, truncus arteriosus repair, VSD
Source: Society of Thoracic Surgeons (STS) National Database 2017
Interventions by Type
2017
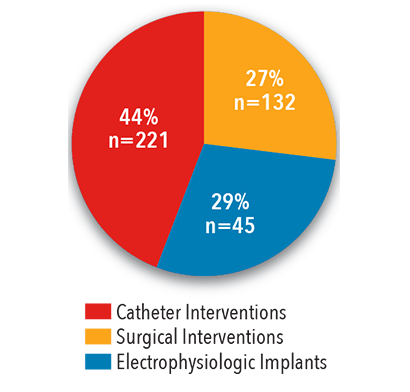
Source: NewYork-Presbyterian
Atrial Septal Defect Repair
2017
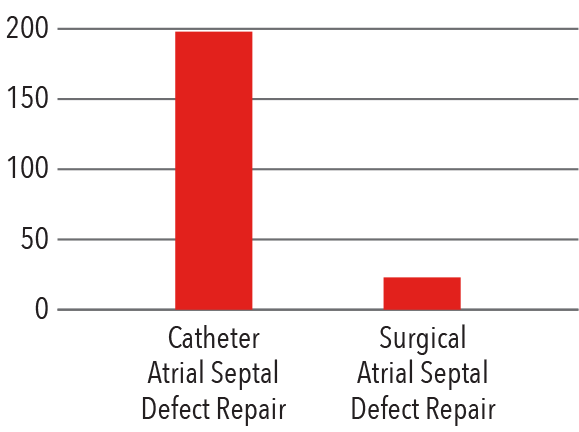
Source: NewYork-Presbyterian
Operative Mortality
2017
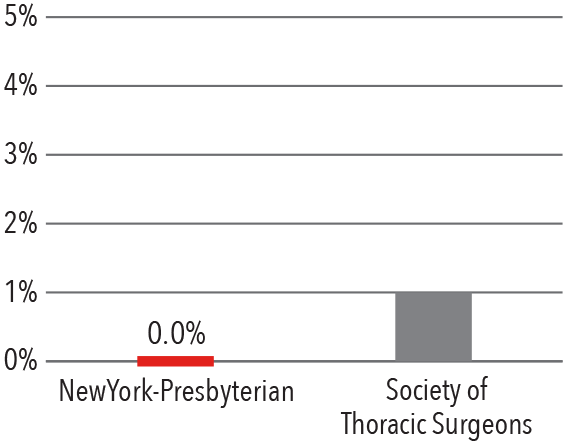
Source: Society of Thoracic Surgeons (STS) National Database
2017
In 2017, NewYork-Presbyterian physicians performed nearly 500 catheter-based, surgical, and electrophysiology implant procedures for adult patients with congenital heart disease.
Examining Advanced Heart Failure in ACHD
Advanced heart failure is becoming increasingly prevalent in the ACHD population. Columbia faculty are at the forefront of examining the impact of heart failure on ACHD patients and are helping to guide a national effort to improve patient outcomes through funded research and team-based clinical care. To this end, they are leading several multicenter research studies. Columbia faculty recently received NIH funding to lead a multicenter study examining the impact of genetics on heart function in patients with complex congenital heart disease. Synergistically, they also received grant funding to study the mechanism of liver disease in patients with a single ventricle and are the lead center on a multinational study to determine which patients with single ventricle physiology should be considered for transplant. Finally, Columbia faculty are collaborating with Amsterdam Medical Center to better identify predictors of systemic right ventricular dysfunction in patients with transposition of the great arteries.
The clinical anomalies of ACHD patients put them at greater risk for poorer outcomes than other patients with advanced heart failure, rendering decisions about treatment more challenging. At NewYork-Presbyterian, collaboration among physicians and surgeons specializing in ACHD and those with expertise in mechanical support and transplant is leading to the development of best practice guidelines for the ACHD population, as well as recommendations for device modifications and alternative therapies.
In an article published in the September-October 2018 issue of Progress in Cardiovascular Diseases, Columbia faculty examined the need to identify which patients are best suited for advanced cardiac therapies, including heart transplantation and mechanical circulatory support, and the timing of these interventions.
Incorporating National Quality Data to Improve Outcomes
NewYork-Presbyterian’s ACHD programs participate in the IMPACT Registry, which collects national quality-focused data on the management and outcomes of pediatric and adult congenital heart disease patients who undergo diagnostic and interventional catheterizations. These procedures include closures for atrial septal defect and patent ductus arteriosus, and transcatheter valve procedures. The comprehensive registry enables members to have access to enchmark data and clinical research that is improving outcomes for adults who have survived a congenital heart disease. Using data from the IMPACT Registry, Columbia faculty published outcomes of pulmonary artery stenting in the March 22, 2016, issue of the Journal of American College of Cardiology.
Collaboration among physicians and surgeons specializing in ACHD and those with expertise in mechanical support and transplant is leading to the development of best practice guidelines.
Novel Therapeutics
Ozaki Aortic Valve Repair
Cardiac surgeons at NewYork-Presbyterian are now performing Ozaki aortic valve repair as an alternative to the Ross procedure. With the Ozaki approach, the diseased aortic valve leaflets are removed, and a new aortic valve is recreated by sewing the leaflets into the native aortic area, providing a new functioning valve. These leaflets may be created from a patient’s own pericardium tissue, which is the preferred option. This offers a number of benefits:
- using native leaflets avoids using a mechanical or synthetic bioprosthetic
- the size and shape of the leaflets provide the valve with the potential to expand as the heart grows and still maintain its ability to function as a valve, which is particularly relevant in pediatric cases
- it is confined to the aortic valve without affecting a structurally normal pulmonary valve that creates, in effect, a two-valve issue for the patient going forward
- the procedure does not preclude performing a Ross procedure at a later time
- it takes less time to perform than the Ross procedure, and patients spend less time onbypass
While the Ozaki procedure is not suitable for every patient with aortic valve disease, it provides another, more patient-specific option for surgical therapy.
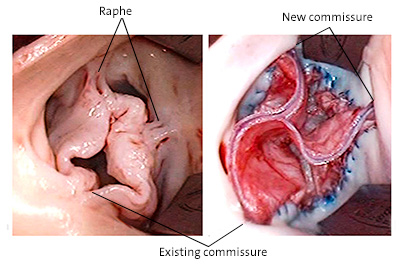
Operative view of pre- and post-tricuspid repair of unicuspid aortic valve in a 14-year-old boy



