Coronary Artery Disease
A Destination for Complex Coronary Artery Disease
NewYork-Presbyterian is a major destination for patients with the most critical heart conditions who have exhausted all other avenues of care. Here, they find an array of treatment alternatives provided by heart teams comprised of cardiologists, interventionalists, and cardiac surgeons. These patients today are older and present with a more significant burden of atherosclerotic disease and comorbid conditions. Many have undergone intensive medical therapy with prior procedures but continue to have progression of disease, in-stent restenosis, or graft failure. Some have been told that there are “no options” for them.
Another category of complex patients is those with poor ventricular function (weak hearts due to prior heart attacks or progressive disease). For these seriously ill patients, our cardiac specialists can intervene with circulatory support devices, including the Impella heart pump, extracorporeal membrane oxygenation (ECMO), or intra-aortic balloon pump.
Meeting the Challenge of Chronic Total Occlusions
Chronic total occlusions have historically been one of the most challenging types of blockages to treat with an interventional procedure. At NewYork-Presbyterian, specialists in complex coronary and peripheral vascular interventional procedures are achieving success rates as high as 90 percent with CTO percutaneous coronary intervention (PCI). Columbia researchers recently took part in a study of in-hospital outcomes when performing more than one CTO-PCI during the same procedure, the results of which were published in the August 1, 2018, issue of the American Journal of Cardiology. The investigators compared the clinical and angiographic characteristics and procedural outcomes of 2,955 patients who underwent treatment of single versus >1 CTO during the same procedure in 20 global centers.
More than one CTO lesion was attempted during the same procedure in 58 patients and 70 percent of them were located in different major epicardial arteries. The multi-CTO-PCI group had higher risk of in-hospital mortality and stroke, longer procedure duration, and higher radiation dose. The investigators concluded that staged revascularization may be the preferred approach in patients with >1 CTO lesion requiring revascularization, as treatment during a single procedure was associated with higher risk for periprocedural complications.
The Case for All Arterial Revascularization
NewYork-Presbyterian’s cardiothoracic surgeons are increasingly using all arterial revascularization, including bilateral mammary and radial artery grafts, supported by evidence that shows arterial revascularization leads to more enduring outcomes. Weill Cornell faculty contributed to a meta-analysis looking at mortality rates when comparing arterial conduits (AC) to great saphenous vein grafts (GSV) as a third conduit for revascularization of the right coronary artery system, in addition to the bilateral internal mammary artery on the left coronary artery. Analyzing data on 4,121 patients, the researchers found ACs were significantly associated with lower long-term mortality rates. Comparisons between the GSV and either the right gastroepiploic artery or the radial artery showed similar results. Their findings were published in the January 12, 2019 online issue of the European Journal of Cardiothoracic Surgery.
A multicenter international study led by Weill Cornell faculty looked at three conduits — the radial artery (RA) versus the right internal thoracic artery (RITA) versus the saphenous vein (SV) — as the second-best conduit after the internal thoracic artery for CABG. Prior to the study, no network meta-analysis had compared these three strategies. The researchers looked at all-cause long-term mortality in nearly 150,000 patients, concluding that the use of the RA or the RITA was associated with a similar and statistically significant long-term clinical benefit compared with the SV. There were no differences in operative risk or complications between the two arterial conduits.
Acute Myocardial Infarction
NewYork-Presbyterian performed more than 3,200 PCI procedures in 2017, with a 97.8% angiographic success rate.
STEMI Performance Measures
2017
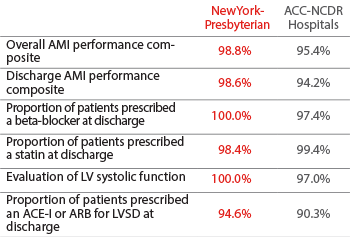
Source: American College of Cardiology National Cardiovascular Data Registry (ACTION Registry®-GWTG™) / Institutional Outcomes Report 2017
Percutaneous Coronary Intervention
Risk Factors of Patients Undergoing PCI
2017

Source: American College of Cardiology National Cardiovascular Data Registry (ACC-NCDR) CathPCI Registry Institutional Outcomes Report 2017
All Adverse Events*
2017
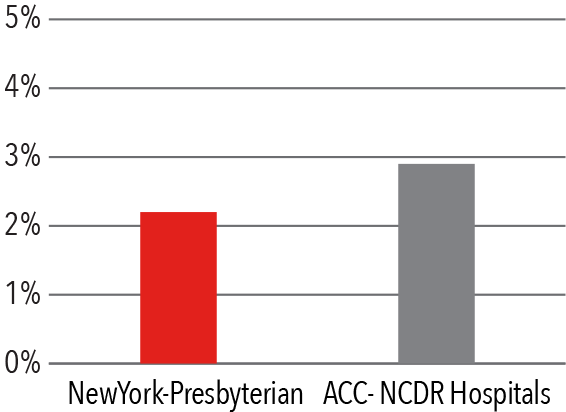
* Composite of adverse events — death, emergency CABG, stroke, repeat target vessel revascularization Source: American College of Cardiology National Cardiovascular Data Registry (ACC-NCDR) CathPCI Registry Institutional Outcomes Report 2017
Mortality
2017

Source: American College of Cardiology National Cardiovascular Data Registry (ACC-NCDR) CathPCI Registry Institutional Outcomes Report 2017
Coronary Artery Bypass Grafting
Volume
2017

Source: NewYork-Presbyterian
30 day Mortality
July 1, 2014 - June 30, 2017

Source: Hospital Compare (of 1,194 hospitals in the U.S.)
Isolated CABG Complications
2017
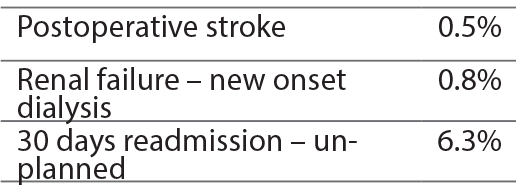
Source: Vizient Clinical Data Base/Resource Manager™ used by permission of Vizient. All rights reserved.
Isolated CABG Mortality
2017
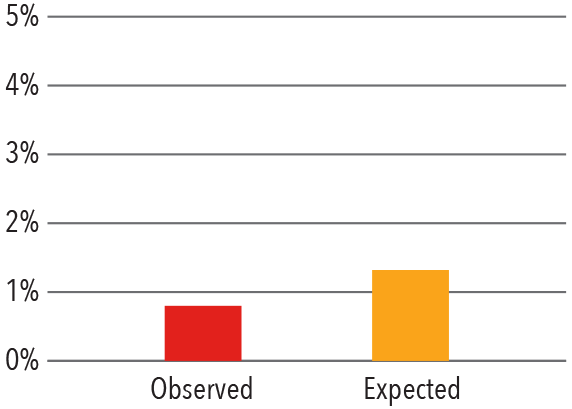
Source: Vizient Clinical Data Base/Resource Manager™ used by permission of Vizient. All rights reserved.
Novel Therapeutics
Hybrid Coronary Revascularization: Best of Both Worlds
Columbia surgeons continued to push the boundaries of surgical treatment for coronary artery disease with the exploration of hybrid coronary revascularization (HCR), which enables surgeons to provide a combination of therapies for patients with multivessel disease. HCR combines minimally invasive surgical coronary artery bypass grafting of the left anterior descending artery with percutaneous coronary intervention (PCI) of non-left anterior descending vessels. The hybrid revascularization approach evolved from a consensus that the most important bypass in terms of longevity and success is the left internal mammary artery (LIMA) to the left interior descending artery (LAD) bypass, which can be accomplished robotically without the heart-lung machine and without an incision, or with a limited access, minimally traumatic approach. Stents are substituted for saphenous vein grafts for non-LAD lesions.
Columbia surgeons were among the first in the country to offer this hybrid approach, and they are currently co-principal investigators in the NIH-sponsored multicenter randomized Hybrid Coronary Revascularization Trial comparing hybrid coronary revascularization to conventional percutaneous coronary intervention. The primary objective is to determine whether the hybrid approach is associated with a reduction in major adverse cardiac and cerebrovascular events compared to PCI with drug-eluting stents. The trial also seeks to determine the impact of HCR compared to PCI on health status and quality of life. The ability to deliver a new therapy for coronary artery disease that provides durability, but without the trauma and prolonged recovery time characteristic of conventional CABG, would be a major advance in the field of cardiovascular medicine. The study, which began enrollment in 2017, will continue to 2024.



