Hypertrophic Cardiomyopathy
Integrated and Comprehensive Care
NewYork-Presbyterian calls on the multidisciplinary skills of cardiologists, cardiovascular imaging specialists, surgeons, electrophysiologists, and geneticists to offer patients the full range of treatment modalities for the management of hypertrophic cardiomyopathy (HCM), the most common genetic cardiovascular disease affecting one in 500 individuals.
Patients are offered genetic counseling and testing, a standard practice not readily available outside of a large university setting. Columbia researchers maintain a biorepository of genetic information with the Columbia Precision Medicine Initiative for the purposes of identifying new genes related to the development of HCM. Any patient with HCM is systematically offered screening for first-degree relatives.
Virtual Septal Myectomy Aids Preoperative Planning
While septal myectomy is the preferred treatment for patients with obstructive hypertrophic cardiomyopathy refractory to medical therapy — and routinely performed at NewYork-Presbyterian as the least-invasive surgical approach — it is a challenging procedure that relies on a surgeon’s subjective assessment through a limited transaortic surgical view. The mainstay of preoperative imaging assessment remains transthoracic echocardiography, though this modality can significantly mislead in preoperative assessment with regards to location and severity of left ventricle thickness. To address this, Columbia and Weill Cornell cardiologists and cardiac surgeons have developed a virtual myectomy (VM) technique using 3-dimensional reconstruction of gated cardiac CT to assist the intraoperative objective assessment of the adequacy of the resection.
In a retrospective study, the results of which were published in the Journal of Thoracic Cardiovascular Surgery in November 2018, the researchers reviewed 15 patients who underwent a septal myectomy guided by preoperative virtual myectomy between March 2016 and July 2017.
Using gated cardiac CT with 3D reconstruction, they were able to reproduce the appearance of the heart under cardioplegia in diastolic arrest; 100 percent of relevant surgical landmarks in all patients were seen preoperatively. Postoperative discussions indicated that preoperative virtual myectomy was helpful in determining how much myocardium to resect as well as clarifying surgical landmarks and anatomy during septal myectomy. Other benefits included detailing the regional difference of septal thickness and width of the “septal band.” The Weill Cornell and Columbia physicians believe this also contributed to achieving a satisfactory clinical outcome.
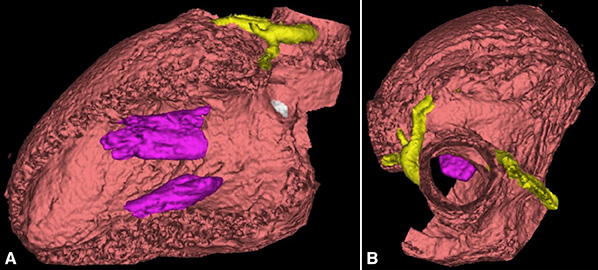
3D reconstruction of the left ventricle with (A) lateral wall removed to visualize septum and (B) surgical transaortic view
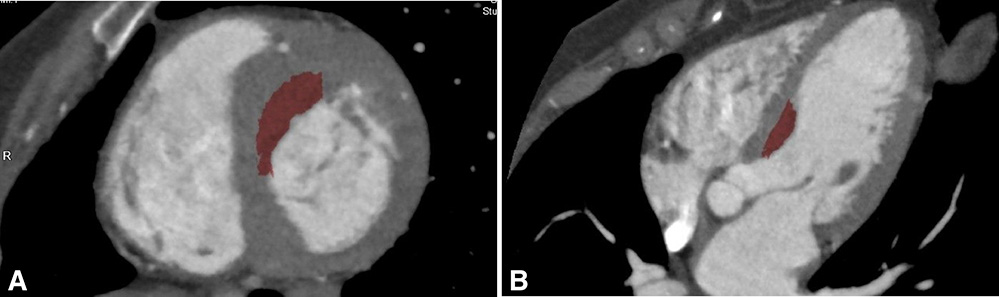
Area of planned myectomy (red) is visualized on the (A) short axis and (B) long-axis views of left ventricle/right ventricle on gated CT.
The endoscopic robotic septal myectomy with large patch augmentation of the anterior mitral valve leaflet is a radical change in paradigm. Preliminary results of this novel approach are promising.
Novel Therapeutics
Robotic Septal Myectomy
While the standard surgical septal myectomy is performed via sternotomy, NewYork-Presbyterian/Weill Cornell offers a totally endoscopic robotic procedure that allows for both septal myectomy and augmentation of the anterior leaflet. The many potential advantages to this minimally invasive approach include exquisite visualization of the septum from the aortic valve to the apex of the heart. The endoscopic robotic approach also allows for easier access to mitral valve subchordal structures and the avoidance of residual postoperative gradients due to inadequate myectomy by enlarging both sides of the left ventricular outflow tract (LVOT).
Mitral valve abnormalities are a key feature of hypertrophic obstructive cardiomyopathy. Early in systole, the anterior leaflet of the mitral valve is one-half of the LVOT. In the robotic approach, surgeons insert a patch that essentially works as an LVOT enlargement maneuver by moving the anterior leaflet into a horizontal position early in systole and away from the septum.
The endoscopic robotic septal myectomy with large patch augmentation of the anterior mitral valve leaflet is a radical change in paradigm. Preliminary results of this novel approach are promising. In a review of 26 patients with a mean septal thickness of 22.3+5.3cm, all patients had systolic anterior motion and mean LVOT gradient 128.2+38.99mmHG. There were no deaths postoperatively, no systolic anterior motion in any patients, and the mean LVOT gradient was in single digits.
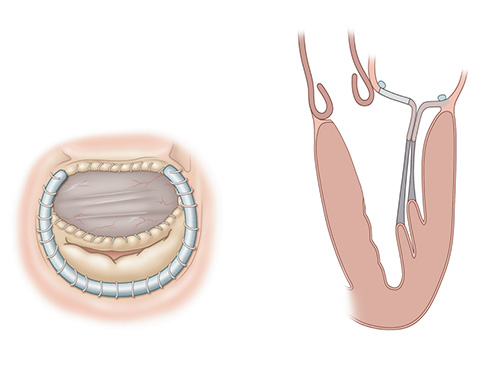
Robotic septal myectomy with anterior leaflet patch. (A) postoperative heart — superior view (B) postoperative heart — long axis view
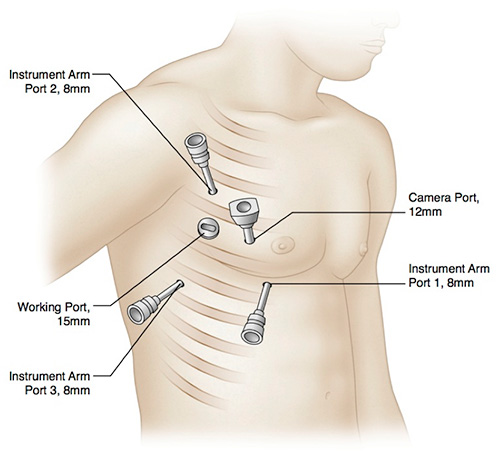
Totally endoscopic robotic septal myectomy ports



