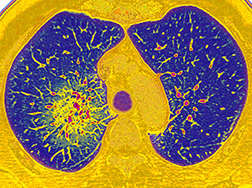
Pulmonary Hypertension
The Pulmonary Hypertension Centers of NewYork-Presbyterian are among the largest programs in the world for pulmonary hypertension, caring for patients with idiopathic and heritable pulmonary hypertension and those with medical conditions that predispose them to its development. Accredited by the Pulmonary Hypertension Association as Pulmonary Hypertension Centers of Comprehensive Care, the Heart Failure and Pulmonary Hypertension Services in the Perkin Center for Heart Failure of NewYork-Presbyterian/Weill Cornell Medical Center and the Pulmonary Hypertension Comprehensive Care Center of NewYork-Presbyterian/Columbia University Irving Medical Center manage some of the most complicated and sickest patients with this rare, progressive cardiopulmonary disease.
Creating In-Depth Multidisciplinary Partnerships
In treating all forms of pulmonary hypertension, our cardiologists form relationships with multiple specialties to comprehensively manage and address patients’ specific needs. As one example, a cardio-renal hemodynamics team supports the efforts of the pulmonary hypertension and heart failure team. Our specialists also work closely with oncologists in the evaluation and management of patients with cancer, as there is an increasing appreciation of aspects of pulmonary hypertension as sequela of not only the disease, but also of treatments of various malignancies. Collaborations with pulmonologists are exploring possibilities for the treatment of pulmonary hypertension secondary to lung disease, a population of patients who do not have good treatment options outside of supportive lung care.
Managing Pulmonary Hypertension and Heart Failure
Pulmonary hypertension and right heart failure complicate the management of about one-third of the patients with heart failure. Our cardiologists provide management strategies for all aspects of pulmonary hypertension, be they idiopathic or hereditary; connective tissue disease; congenital heart disease-associated PAH [WHO Group 1]; or a consequence of left-sided heart disease, such as heart failure reduced or preserve ejection fraction, cardiomyopathy, or valvular heart disease; lung or hypoxic related; or chronic thromboembolic disease related pulmonary hypertension. The nuances and subtleties involved in advanced heart failure require the expertise of a multidisciplinary, collaborative center.
Identifying the optimal timing of therapeutic interventions is critical. Our cardiologists understand what technologies and therapies are appropriate for each patient and when to apply them. For example, this includes when to move on to mechanical assist devices or heart transplantation for heart failure and lung transplantation for pulmonary hypertension if more conventional high-risk cardiac surgery or catheter-based procedures are no longer possible.
Offering Advanced Therapeutic Options
Our centers provide medical, interventional, and surgical management of pulmonary hypertension and vascular disease, including catheter-directed fibrinolytic therapy, pulmonary embolectomy, and pulmonary thromboendarterectomy.
Working closely with medical and surgical ECMO teams, our physicians are pursuing mechanical solutions for patients with pulmonary hypertension as a bridge to high-risk surgery or transplant. By using novel configurations of ECMO, patients who previously had sudden catastrophic pulmonary hypertensive crises can now be managed safely through to transplant, if required. Mechanical support has enabled some patients with pulmonary hypertension to undergo elective surgeries such as hip replacement, as well as gall bladder and thyroid surgery. Our medical and surgical team was also among the first to perform a palliative unidirectional valved Potts shunt in an adult with severe idiopathic pulmonary arterial hypertension.
Pursuing Research Endeavors
In 2014, the National Heart, Lung and Blood Institute launched the PVDOMICS (Redefining Pulmonary Hypertension through Pulmonary Vascular Disease Phenomics) program with additional funding from the Pulmonary Hypertension Association to augment the current pulmonary hypertension classification based on shared biological features of 1,500 participants. Columbia and Weill Cornell serve as two of the seven clinical centers across the country to carry out the study, which continues to recruit patients.
Weill Cornell clinicians currently serve as principal investigators in a multicenter clinical trial for patients with interstitial lung disease and pulmonary hypertension, a unique study offering patients treatment with an inhaled pulmonary vasodilator, treprostinil, and evaluating efficacy of this drug in a patient population that has never been looked at before.
Pulmonary arteritis, a rare cause of pulmonary hypertension
A number of patients with pulmonary hypertension have rheumatological- based and inflammatory pulmonary, vascular, and cardiac disease. Investigators at Hospital for Special Surgery, which is affiliated with Weill Cornell, and Columbia are participating in a multicenter clinical trial sponsored by the National Institute of Allergy and Infectious Diseases to evaluate the effectiveness of rituximab for scleroderma-associated pulmonary arterial hypertension. The phase 2 study seeks to determine if rituximab changes the resistance in lung blood vessels in patients with systemic sclerosis (SSc) as measured by right heart catheterization after 24 weeks of treatment. A substudy is evaluating the therapeutic effect of rituximab on the right ventricle of patients with SSc-PAH as determined by cardiac MRI.
Columbia is one of only four centers in the country participating in the TROPHY 1-US (Treatment of Pulmonary Hypertension 1-US) clinical trial, which is evaluating pulmonary artery denervation using the Therapeutic Intra-Vascular UltraSound (TIVUS™) System to improve functional capacity, hemodynamics, and overall effectiveness in patients with pulmonary arterial hypertension.
Novel Therapeutics
Managing CTEPH
Chronic thromboembolic pulmonary hypertension (CTEPH), a rare and progressive form of pulmonary hypertension, results from the incomplete resolution of acute pulmonary emboli that forms fibrotic material. This scar-like tissue disrupts circulation and prevents blood flow to the lungs. The leading symptoms of CTEPH are shortness of breath and fatigue, which can be difficult to diagnose since they are common symptoms of many other pulmonary conditions.
NewYork-Presbyterian’s multidisciplinary CTEPH programs provide medical management, including anticoagulation therapy or pulmonary vasodilators. The Hospital is also one of the few sites in the country to provide balloon pulmonary angioplasty for patients who are not candidates for surgery, resulting in both hemodynamic and functional benefits.
Our cardiothoracic surgeons also offer highly specialized expertise in pulmonary thromboendarterectomy (PTE), a complex and challenging surgery to remove the chronic thromboembolic disease. PTE, which has been shown to be the best treatment in extending a patient’s survival, requires careful patient selection, a surgical skill set, and a high level of postoperative medical care and management.



