Adult Congenital Heart Disease
NewYork-Presbyterian’s dedicated adult congenital heart disease programs assure that this population receives comprehensive management and the highly specialized clinical services mandated by the complexity of their medical and surgical histories. A multidisciplinary approach – including specialists in pulmonary hypertension, heart failure, electrophysiology, and cardiac imaging – is used to manage atypical presentations of heart disease that will frequently require surgical or interventional procedures.
Our cardiologists, interventionalists, and cardiac surgeons offer advanced expertise and experience in all the major procedures for PFO, PDA, or VSD closure, transcatheter valve replacement for both pulmonary and tricuspid valves, and stenting of pulmonary arteries and coarctation of the aorta.
Advancing Catheter-Based and Surgical Approaches
In 2016, our adult congenital heart disease team performed nearly 400 surgical, catheter-based, and electrophysiology implant procedures in patients with adult congenital heart disease.
-
Traditional surgical techniques are still the standard of care for patients in basically good health, but who often need valve surgery. Our surgeons are now leveraging the advantages of the less-invasive, catheter-based approaches for adult congenital heart disease patients, such as Fontan patients, who present with more complicated comorbidities associated with their heart condition and therefore may not be candidates for open heart surgery. These include transcatheter aortic valve and percutaneous mitral and tricuspid valve procedures.
-
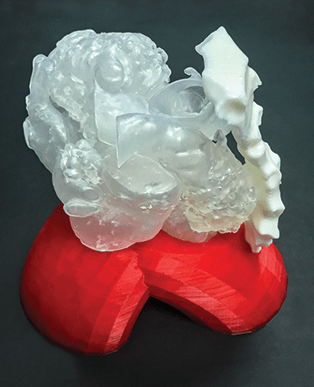
Our surgeons are using ventricular assist devices for adult congenital heart disease patients who progress to end-stage heart failure. Complex anatomy of these patients makes it particularly challenging for placement of these devices. Our surgeons are applying advanced cardiac MRI and CT for 3-D printing technology to help plan surgery and optimize outcomes with the goal of using ventricular assist devices as a destination therapy.
-
Researchers at Weill Cornell are participating in the AMPLATZERTM PFO Occluder Post-Approval Study for patients with PFO closure in cryptogenic strokes.
-
Our physicians are also beginning to evaluate 4-D flow, a new technique in cardiac MRI, to help predict the timing of surgery for tricuspid regurgitation in Ebstein’s anomaly and to determine if it is a more accurate method than echocardiography for assessing aortic valve regurgitation in preparation for patients undergoing heart surgery. The approach may prove useful when echo images are insufficient or when a discrepancy exists between the echocardiogram and the clinical presentation.
Case Study
A 40-year-old woman was born with double outlet right ventricle and pulmonary stenosis and underwent a Rastelli operation at five years of age. At 18 years old, she required a replacement RV-PA conduit, however, this procedure was abandoned because of the severe complexity of the surgery. She was left with severe pulmonary regurgitation. She was seen at two major medical centers in New Jersey and Pennsylvania but was unable to be offered definitive treatment due to the complexity of her case. She saw the ACHD team at NewYork- Presbyterian for a third opinion and underwent placement of a Melody transcatheter pulmonary valve replacement. She improved a little, however, she continued to have congestive heart failure and hypoxemia due to severe tricuspid stenosis and severe subaortic stenosis.
Due to her unusual anatomy and very high surgical risk, our ACHD team, along with the cardiac imaging team, created a 3-D printed reconstruction of her heart. We used this to plan a complex repair, rarely used in adults, by making a homograft right atrial to right ventricular connection, bioprosthetic pulmonary valve replacement, and resection of the subaortic stenosis. This surgery was long and complex, however, the patient had an excellent result with no complications.
Managing Noncardiac Complications
-
Our physicians are establishing and refining care pathways for patients with Fontan single ventricle anatomy who are prone to liver complications, working closely with hepatology colleagues.
-
In collaboration with colleagues in pulmonary hypertension, congenital heart disease specialists are participating in an NIH study on patients with Eisenmenger’s syndrome, specifically looking at patients with atrial septal defects and pulmonary hypertension.
-
Development of a formal program for women with congenital heart disease who are undergoing high-risk pregnancies is underway, bringing together specialists in maternal-fetal medicine, cardiology, and anesthesia to manage a detailed plan for delivery and postpartum care.
Adult Congenital Heart Surgery
2016
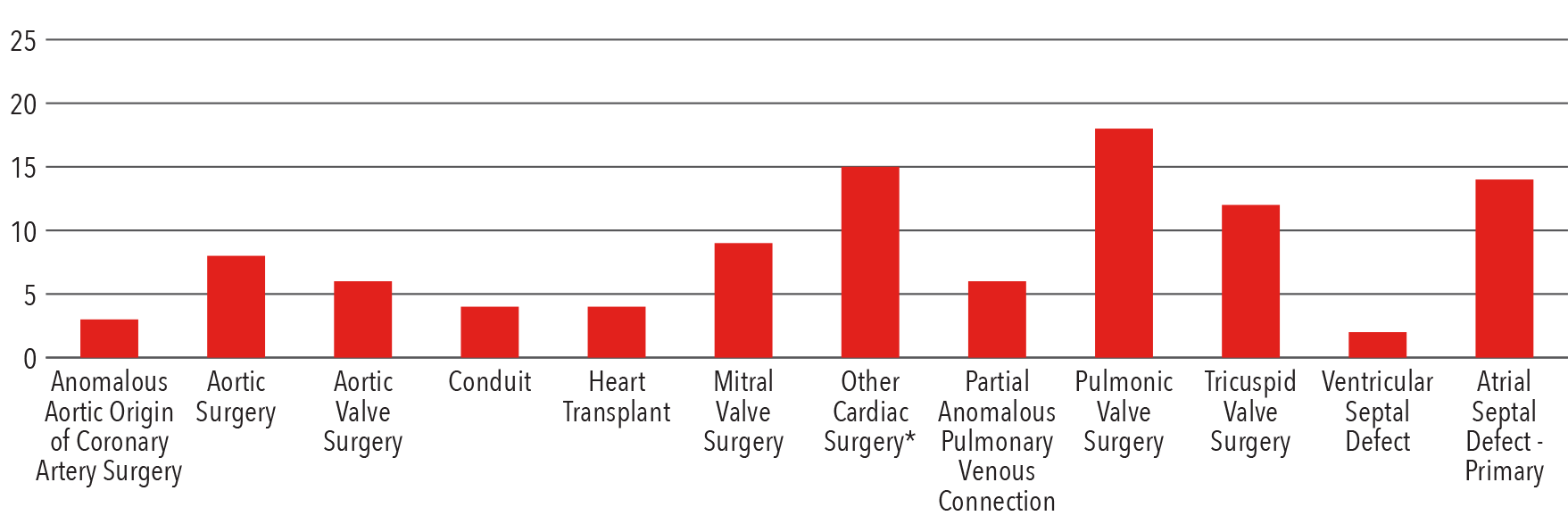
*Other cardiac surgery: Fontan, Right Ventricular Outflow Tract Procedure, Maze, Cone Procedure, PMI,
Pulmonary Arterial Reconstruction, Cor Triatriatum Repair, Mediastinal Procedure, Sternal Wire Removal
Source: Society of Thoracic Surgeons (STS) National Database 2016
Interventions by Type
2016
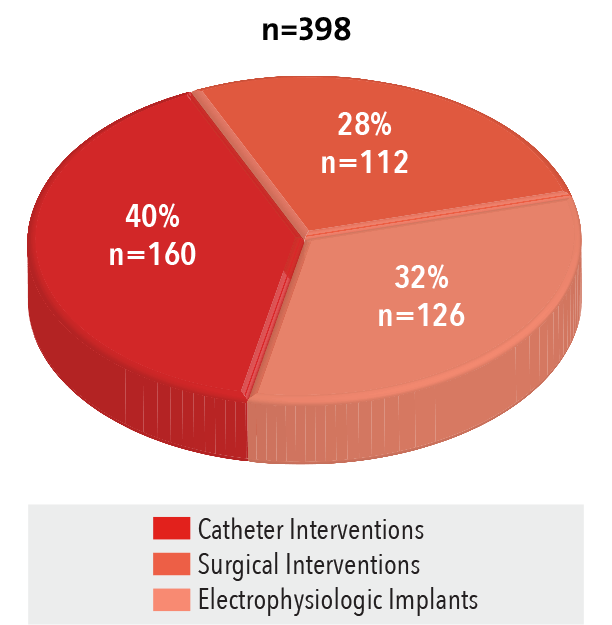
Source: NewYork-Presbyterian
Atrial Septal Defect Repair
2016
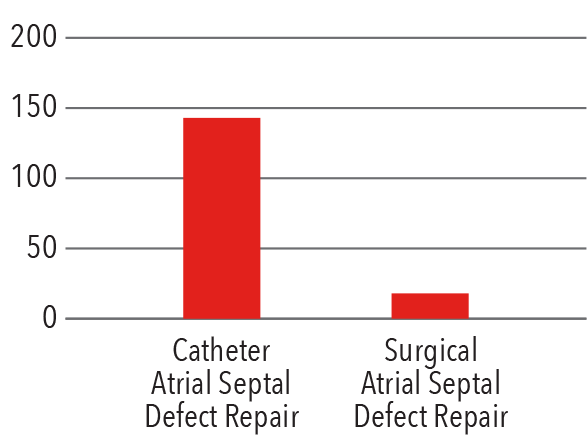
Source: NewYork-Presbyterian



