Arrhythmias
Fluoroless Catheter Ablation of Atrial Fibrillation
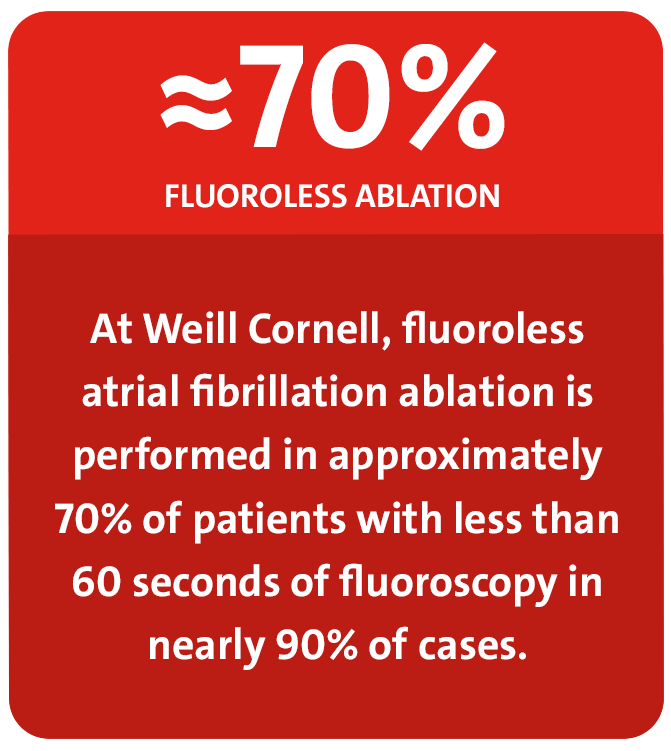
Traditionally, physicians have primarily used fluoroscopy to navigate catheter positioning for mapping and ablating atrial fibrillation. NewYork-Presbyterian is among the leading hospitals in the country to perfect the ability to map and ablate arrhythmias with three-dimensional intracardiac echocardiography. This minimally invasive imaging modality allows for real-time image guidance and visualization of anatomical structures without ionizing radiation, allowing our physicians to manipulate catheters to treat atrial fibrillation without exposing patients or the electrophysiologist to any appreciable amount of fluoroscopy.
The vast majority of our patients with atrial fibrillation do not require fluoroscopy. However, there are challenges in patients with preexisting pacemaker and defibrillator leads, those with atrial septal defect closure devices, and those with anatomic anomalies or poor acoustic windows. In these circumstances, since safety is always the highest priority, short flashes of fluoroscopy may be appropriate.
Electrophysiology Procedures
2016
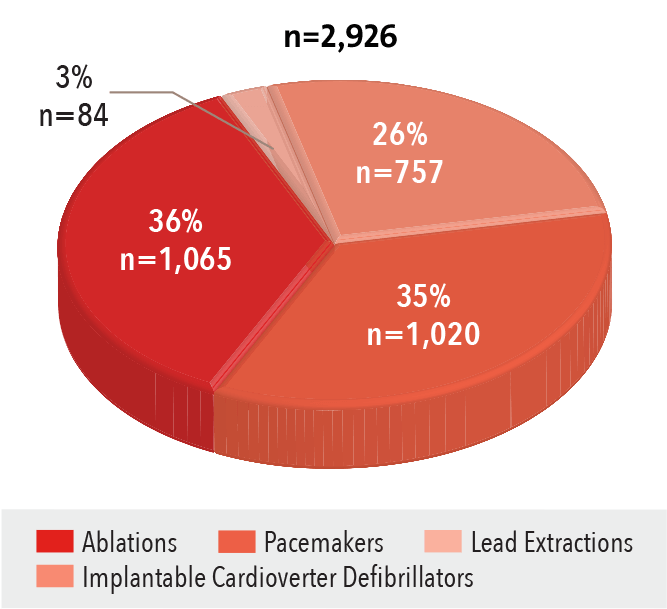
Source: NewYork-Presbyterian
Tracking of the Transseptal Sheath
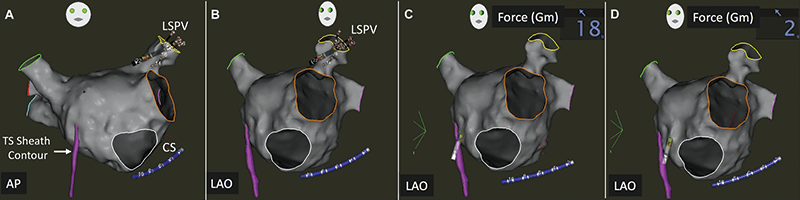
Acquisition of right atrial anatomy during insertion of the ablation catheter through the transseptal sheath allows for its position to be annotated on the FAM map or merged CT scan. This facilitates fluoroless reintroduction of the ablation catheter and sheath into the left atrium in cases where transseptal access is inadvertently lost.
Advanced Left Ventricular Leadless System
NewYork-Presbyterian is among the first institutions in the United States to test a wireless, endocardial pacing system for stimulating the left ventricle in patients with heart failure who require cardiac resynchronization therapy. The system uses a proprietary wireless technology to deliver pacing stimulation directly to the inside of the left ventricle of the heart. This approach is designed to overcome limitations of existing cardiac resynchronization therapy systems that deliver pacing stimulation to the outside of the left ventricle. Pacing from the inside of the left ventricle is believed to be more physiologic.
Research Highlights
Electrocardiographic Findings in NBA Athletes
Columbia researchers, in partnership with the National Basketball Association, served as lead authors on an observational study looking at ECG data for NBA athletes. The results, published in the December 6, 2017, issue (Epub) of JAMA Cardiology, showed that the prevalence of abnormal ECG findings in NBA players is higher than in other studied athlete groups. While athlete-specific international criteria improved ECG specificity over previous ECG interpretation criteria in these players, abnormal ECG classification remained high. Additionally, the development of left ventricular concentric remodeling appears to have a significant influence on the prevalence of abnormal ECG classification and repolarization abnormalities in this elite athlete population. Continued work is required to investigate the significance of these findings.
Navigation-Guided versus Manual Catheter Ablation
Weill Cornell researchers conducted a study comparing the outcomes of robotic magnetic navigation-guided ablation with manual ablation of ventricular arrhythmias from the left ventricular and right ventricular papillary muscles. Catheter ablation was initially performed using robotic magnetic navigation guidance in 24 patients and manual guidance in 11 patients. The researchers concluded that the use of the robot magnetic navigation-guided approach to target papillary muscle ventricular arrhythmias results in comparable success rates seen with manual ablation, but with lower fluoroscopy times and decreased use of transaortic retrograde access.
Enhancing Assessment of Electromechanical Behavior
Columbia researchers looked at the value of electromechanical wave imaging (EWI) in the assessment of heart failure patients and cardiac resynchronization therapy (CRT). This noninvasive, ultrasound-based technique can map electromechanical activity at high spatial and temporal resolution and with real-time feedback. In their investigation, the results of which appeared in the January 2017 issue of Pacing and Clinical Electrophysiology, the researchers concluded that EWI was capable of characterizing local cardiac electromechanical behavior as it pertains to heart failure and CRT response. Activation sequences obtained with EWI allow for quantification of LV lateral wall electromechanical activation, thus providing a novel method for CRT assessment.
Reconstructing Scar Areas
Researchers at Weill Cornell sought to compare areas of scar marked on 3-D integrated intracardiac echocardiogram (ICE) with abnormal electrogram sites in patients with cardiomyopathy and ventricular tachycardia (VT). They concluded ICE delineation of scar regions is feasible and shows excellent correlation with low voltage regions, as well as local abnormal ventricular activities in normal voltage regions. Image integration of scar areas into the anatomic mapping system can help focus attention to areas of interest for substrate mapping during VT ablation.
Catheter Ablations
Volume
2012-2016
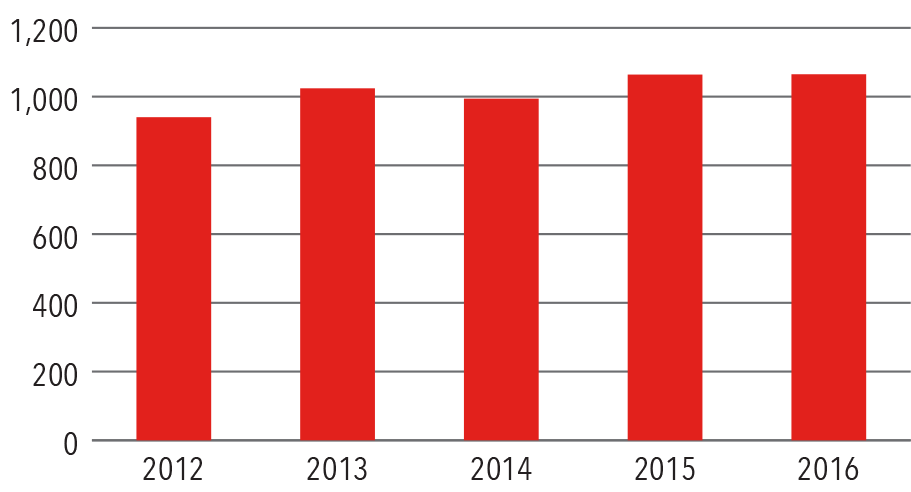
Source: NewYork-Presbyterian
By Type of Arrhythmia
2016
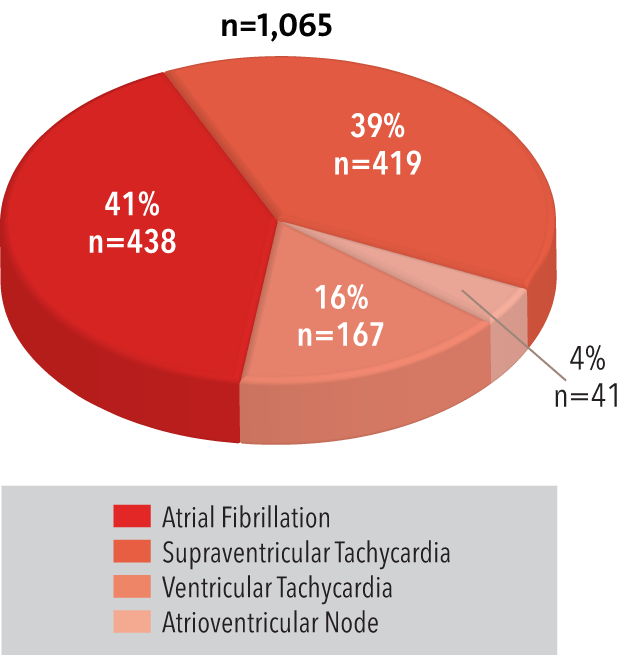
Source: NewYork-Presbyterian



