Pulmonary Hypertension
NewYork-Presbyterian’s Pulmonary Hypertension Centers, which are accredited by the Pulmonary Hypertension Association as Pulmonary Hypertension Centers of Comprehensive Care, are among the largest programs in the world for chronic thromboembolic pulmonary hypertension (CTEPH). Our physicians manage the most complex and sickest patients with idiopathic and heritable pulmonary hypertension and pulmonary hypertension related to diseases of the connective tissue, congenital heart and left heart disease, and lung, hematological, oncologic, and renal and hepatic diseases.
PVDOMICS Study Group
NewYork-Presbyterian is one of six centers to participate in the PVDOMICS (Redefining Pulmonary Hypertension through Pulmonary Vascular Disease Phenomics) study group launched by the National Heart, Lung and Blood Institute, which seeks to improve understanding of pulmonary vascular disease through phenomics. The group’s aim is to augment the current pulmonary hypertension classification based on shared biological features of the 1,500 participants with pulmonary hypertension and disease and those who are healthy comparators. The phenomic data generated is expected to be a rich resource to heart and lung disease investigators seeking to identify therapeutic targets.
Advanced Therapeutic Options
Through multidisciplinary partnerships, our centers are able to offer medical, interventional, and surgical management of pulmonary hypertension and vascular disease, including catheter-directed fibrinolytic therapy, pulmonary embolectomy, and pulmonary thromboendarterectomy.
-
In collaboration with the Pulmonary Embolism Response Team program, we continue to expand treatments for chronic thromboembolic pulmonary hypertension utilizing balloon pulmonary angioplasty.
-
Working closely with medical and surgical ECMO teams, our physicians are pursuing mechanical solutions for patients with pulmonary hypertension as a bridge to high-risk surgery or transplant. This mechanical support has enabled some of our patients to undergo such elective surgeries as hip replacement, as well as gall bladder and thyroid surgery. Most recently, they assisted in the management of a successful pregnancy of a patient with Eisenmenger’s syndrome, from delivery through recovery.
-
NewYork-Presbyterian is one of the few sites in the country providing the newer option of balloon pulmonary angioplasty for CTEPH, particularly for patients who are not candidates for pulmonary thromboendarterectomy (PTE). The procedure offers both hemodynamic and functional benefits.
-
Our medical and surgical team was among the first to perform a palliative unidirectional valved Potts shunt in an adult with severe idiopathic pulmonary artery hypertension. (See case study, page 17.)
Research Investigations
-
Leaders in the field of genetic discovery in cardiovascular disease, Columbia researchers have reported the first mutation associated with inherited forms of pulmonary hypertension and have identified three novel genes for the disease.
-
Columbia University Medical Center is one of three centers in the country that will evaluate pulmonary artery denervation, which is performed in the catheterization lab, as a treatment to improve functional capacity, hemodynamics, and overall effectiveness in patients with pulmonary artery hypertension. Recruitment is now open for the trial of the novel approach, which has never been performed before and is made possible by the close collaboration of cardiologists, interventionalists, surgeons, and critical care specialists.
-
The presence of massive uterine leiomyomas has not been widely described as a risk factor for CTEPH, however, pelvic venous congestion may predispose these women to deep vein thrombosis and CTEPH. In a review of seven women with massive uterine leiomyomas and CTEPH, our clinicians in pediatrics, medicine, and obstetrics and gynecology found that women with these co-occurring conditions can safely undergo PTE with the appropriate multidisciplinary team and proper planning for operative placement of an inferior vena cava filter followed by hysterectomy shortly after PTE. The physicians recommend that women with massive fibroids and unexplained dyspnea consider a workup for CTEPH.
Case Study

Schematic illustrating the location and function of the novel modified valved Potts shunt. PAP = pulmonary artery pressure SBP = systolic blood pressure
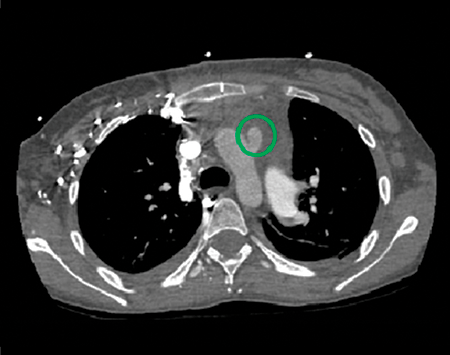
Postoperative mediastinal window showing the location of the modified Potts shunt (green circle).
A 22-year-old woman with a 15-year history of idiopathic pulmonary arterial hypertension (IPAH) remained symptomatic despite balloon atrial septostomy to decrease her risk of resyncope and sudden cardiovascular collapse. Her persistent medication noncompliance and complex social circumstances disqualified her from lung transplantation. Our cardiac team opted to perform a palliative surgical procedure typically reserved for pediatric patients.
The patient presented to an outside hospital with progressive dyspnea of two weeks’ duration after abruptly discontinuing her medications. She was afebrile with an oxygen saturation of 60% while she breathed room air. Her laboratory studies were notable for a brain natriuretic peptide exceeding 3,400 pg/ml and an electrocardiogram demonstrating a stable right bundle branch block. She was started on inhaled iloprost and inhaled nitric oxide and was urgently transferred to NewYork- Presbyterian.
On arrival, she was placed on high-flow nasal cannula and soon thereafter on intravenous epoprostenol, ambrisentan, and sildenafil. A transthoracic echocardiogram revealed a severely dilated right ventricle with poor systolic function, a left ventricular ejection fraction of 35%, and an estimated pulmonary artery systolic pressure of 130 mm Hg.
As the patient was not a candidate for lung transplantation, the decision was made to perform a palliative unidirectional valved Potts shunt – a connection between the main pulmonary artery and the descending aorta – with simultaneous closure of the atrial septostomy. This would effectively generate Eisenmenger’s physiology with a “pop-off” valve from the pulmonary to the systemic circulation, providing right ventricular afterload reduction while maintaining cardiac output and preserving upper body oxygenation. A CT examination of the chest confirmed Potts shunt patency. She was discharged home on postoperative day 21 to take intravenous epoprostenol, ambrisentan, sildenafil, and furosemide. She was anticoagulated with warfarin and aspirin.
Unlike systemic desaturation from atrial-level shunting with a balloon atrial septostomy, the anastomotic sites of a Potts shunt ensure maintenance of fully oxygenated blood flow to the upper body, thereby improving exercise tolerance and reducing the risk of syncope and cardiovascular collapse. Our novel addition of a unidirectional pop-off valve has the benefit of allowing rightto- left shunting during suprasystemic pulmonary hypertensive crises, while preventing left-to-right shunting into the pulmonary artery when pulmonary artery pressure falls below systemic pressure.



