Research
Regenerative Medicine Our innovative studies in the experimental zebrafish model are shedding light on the etiologies of fetal and neonatal cardiac pathology and driving innovations in regenerative medicine. Specifically, researchers are examining how stage-dependent mechanisms that sculpt chamber-specific cardiomyocytes have the potential to improve in vitro generation of ventricular cells, and treat myocardial infarction and congenital heart disease.
AI and Precision Medicine By developing soft robotics-based cardiac compression device technology with soft sensing and soft actuation, our researchers are bringing personalized treatment to children with heart failure.
Valve Disease
Implantable Valve Studies The establishment of NewYork-Presbyterian’s Initiative for Pediatric Cardiology Innovation in 2019 has advanced valve disease translational research including the use of polymers and tissue engineering to create implantable replacement valves that can grow and conform to a child’s anatomy over time. The implantable valves, which are currently being investigated in animal models, can be expanded by noninvasive balloon dilation during cardiac catheterization and may reduce the need for multiple surgeries. Laboratory research is also being conducted on durable heart valve repairs using synthetic materials that mimic the architecture of a normal valve and biocompatible polymers.
Alterra Adaptive Prestent We were among the first in the U.S. to successfully implant the Alterra adaptive prestent as part of an FDA pivotal trial. The Alterra adaptive prestent is a self-expanding, partially covered stent designed to reduce the size of large right ventricular outflow tracts (RVOTs) and provide a landing zone for the SAPIEN 3 transcatheter heart valve. By being able to implant a transcatheter valve in patients with large RVOTs, we reduce the total number of surgeries they may need over their lifetime.
Ozaki Technique Our researchers continue to refine the Ozaki technique where the diseased aortic valve is removed and recreated with leaflet templates made from a tissue substitute taken from the patient’s own pericardium or bovine pericardium.
Norwood Procedure We are examining how the incorporation of a composite valve Sano in the Norwood procedure is improving the growth of the pulmonary arteries and function of the ventricle.
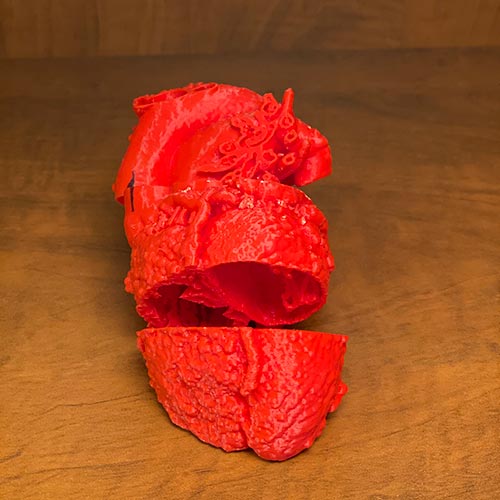
3-D printed heart used for fetal counseling
Novel Imaging
3D Printing We are conducting a multicenter study assessing the utility of 3D printed models for preoperative planning of ventricular assist device placement in patients with congenital heart disease and heart failure. Our recent comprehensive review highlights how 3D printing technology is now increasingly being used to create unique patient-specific models for guidance prior to catheter-based or surgical interventions for patients with heart failure. In 2020, we expanded the use of this technology to generate 3D models for prenatal counseling, aiming to improve parental understanding of CHDs.
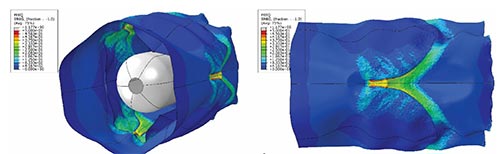
Computational Modeling
In collaboration with computer science engineers our surgical team is working to create patient-specific predictive computational models to 1) help predict when a left ventricle is too small for a biventricular repair and, 2) help to predict the outcomes of a mitral and an aortic valve (including Ozaki technique) repair.
Fetal Interventions
Although supraventricular tachycardia (SVT), including atrial flutter (AF), are the most common causes of intended in-utero fetal therapy, none of the medications used to date have been evaluated in mothers and babies in a randomized controlled clinical trial. Our team is participating in The Fetal Atrial Flutter and Supraventricular Tachycardia (FAST) Therapy Trial, which is a prospective multicenter trial that addresses this knowledge gap and will help to guide therapy for AF and SVT.
Pulmonary Hypertension
Pediatric Pulmonary Hypertension We continue to evaluate the unidirectional-valved shunt as a palliative bridge — an innovative surgical approach that we developed to the classic Potts shunt — in patients with end-stage pulmonary hypertension. We are also assessing novel medical therapeutic approaches for the management of pulmonary hypertension in children.
Pediatric Heart Transplant and Heart Failure
The PumpKIN Clinical Trial As one of 8 vanguard participating sites across the country, the PumpKIN trial will test the safety and efficacy of continuous flow technology in a device designed specifically for smaller children with advanced heart failure (Jarvik 2015). In January 2020, we implanted the fourth Jarvik 2015 in this trial, and subsequently bridged a toddler with dilated cardiomyopathy successfully to heart transplant.
Fontan Circulation We completed the Fontan Udenafil Exercise Longitudinal (FUEL) study and embarked on FUEL-OLE (Open Label Extension) to study the use of udenafil in adolescents with Fontan physiology.
Infantile Cardiomyopathy We are studying genetic variants including the novel MRAS and the RAS signaling pathway in experimental animal models as a potential cause of infantile cardiomyopathy.
Novel Medical Therapeutics
Immunosuppression We are participating in TEAMMATE—a multicenter, randomized trial investigating a novel immunosuppression regimen including everolimus post-heart transplantation.
Pediatric Heart Failure We are participating in the PANORAMA trial, a multicenter, double-blinded trial comparing a novel heart failure medication (entresto) with the established standard of care treatment (enalapril) for pediatric heart failure. The trial includes an open-label long-term extension study on entresto.
Congenital Heart Disease
Pulmonary Vein Stenosis Our researchers created a novel percutaneous animal model of pulmonary vein stenosis using radiofrequency thermal injury. In neonatal swine pulmonary veins, we were able to successfully induce neointimal hyperplasia by thermal injury, which will enable further study of novel interventions for pulmonary vein stenoses.
Disparities in CHD By linking clinical registry and Medicaid data, our researchers are building a state-wide resource to assess longitudinal outcomes and health expenditures, ultimately seeking to identify targets to reduce health inequities among children with CHD.
Surgical Skill Our prospective national survey is examining surgeon-specific patient outcomes and provider characteristics using peer ratings from direct video observation of surgeon technical skills as one possible driver of outcomes for children with CHD.



