Pediatric Cardiomyopathy, Heart Failure, & Transplantation
In 1984, we conducted the world’s first successful pediatric heart transplant in a 4-year-old boy with complex congenital heart disease.
From 2016 to 2019, we performed 104 pediatric heart transplantations, the highest volume in the country.
We were the first in the U.S. to perform an across blood type heart transplant in 2001, and we routinely transplant infants across ABO blood types.
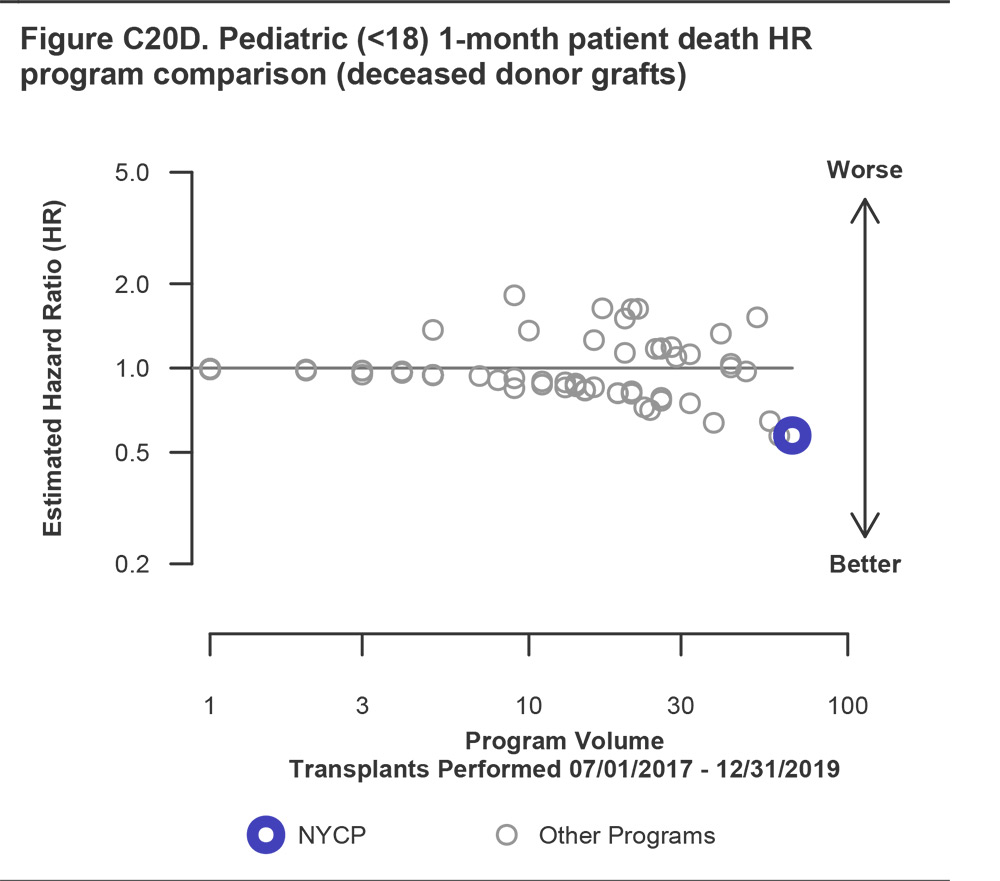
The Program for Pediatric Cardiomyopathy, Heart Failure, and Transplantation began in June 1984 when NewYork-Presbyterian/Columbia surgeons performed the world’s first successful pediatric heart transplant in a 4-year-old boy with complex congenital heart disease. Since that time, the pioneering multidisciplinary transplant team, led for over 35 years by Dr. Linda J. Addonizio, has remained at the forefront of national and international pediatric cardiac transplantation and heart failure efforts. Our transplant program has been consistently ranked in the top 3 nationally in transplant volumes, with outcomes exceeding national and local benchmarks as reported by the Scientific Registry for Transplant Recipients (SRTR).
SRTR User Guide, January 2021
Today, under the direction of Dr. Marc E. Richmond and Dr. Warren A. Zuckerman, NewYork-Presbyterian/Columbia remains one of the largest and most successful pediatric heart transplant centers in North America and the world. Since its inception, our program has pushed the envelope for transplantation in complex congenital heart patients, providing transplants to many children who are turned down by other institutions and programs. From 2016 to 2019, we performed 104 pediatric heart transplantations, which is the most in the United States. Our 1-month, 1-year, and 3-year post-transplant outcomes far exceed the national average (SRTR, 2017-2019).
We specialize in transplanting children with severe pulmonary hypertension, a management protocol that we have been perfecting since the late 1980s, and have devised methods for transplanting children with effective single lung physiology, sparing both of these complex patient populations from a much higher risk heart-lung transplant. We also have extensive experience transplanting patients with failed Fontan physiology with protein losing enteropathy, arteriovenous malformations and/or plastic bronchitis, as well as children with preformed alloantibodies and positive cross-match at transplantation. We were the first in the U.S. to perform an across blood type heart transplant in 2001, and we routinely transplant infants across ABO blood types. Our program is recognized internationally for its excellence in transplant and is a referral center for children from around the world.



