Anterior Hip Replacement
Refining Tools and Techniques to Enhance Outcomes

Dr. Jakub Tatka, Dr. Jeffrey A. Geller, Dr. H. John Cooper, Dr. Alexander L. Neuwirth, Dr. Thomas R. Hickernell, and Dr. Roshan P. Shah
“Anterior hip replacement has been a revolution in hip surgery, making the recovery so much faster, easier, and less worrisome,” says Jeffrey A. Geller, MD, Chief of Hip and Knee Reconstruction at NewYork-Presbyterian/Columbia, whose team of orthopedic surgeons performs the minimally invasive approach virtually 100 percent of the time. “Although both the posterior and anterior approaches have similar outcomes a year out, dramatically improving recovery in the first few months after surgery is a great benefit. Ours is the only hospital in New York where all of our surgeons are skilled in the anterior approach; that’s all we do.”
Traditional hip replacement surgery involves making an incision on the lateral or posterior side of the hip and cutting several different muscles and tendons off of the bone in order to replace the joint. These muscles and tendons then get repaired, but the best studies show that they never again look or act normal. Consequently, this may increase the risk of hip dislocation, one of the leading causes of revision hip replacements. Anterior hip replacement involves a three- to four-inch incision on the front of the hip that allows the joint to be replaced by moving muscles aside without detaching any tendons. Because the tendons and muscles are not detached, patients can return to normal daily activities much quicker after surgery and take fewer pain medications.
“Anterior hip replacements are gaining in popularity every year and now make up over 40 percent of the total hip procedures done in the U.S.,” says H. John Cooper, MD. “There are two variations on the anterior approach – the direct anterior approach and the mini anterolateral Watson-Jones approach. Both approaches are much less invasive than the posterior approach and significantly less disruptive to muscle. And they are associated with the same benefits, including a lower risk of dislocation.”
“Here at Columbia, our surgeons perform both anterior approaches in about equal number,” adds Roshan P. Shah, MD, JD, Director of Complex Adult Hip and Knee Reconstruction. “This enables us to excel in both and compare the two approaches to study their outcomes.”
Optimizing the Anterior Approach
“The anterior approach is driving innovation, including the development of new devices that facilitate implantation with greater accuracy and a decreased risk of perioperative complications, such as fracture and stem subsidence,” says Jakub Tatka, MD. “We have gained such a high understanding of this approach that we are even doing revision surgeries of failed posterior replacements this way.”
“There are emerging technologies, some of which we are using, that incorporate intraoperative images and special algorithms to tell you the exact position of your implants and whether or not you need to alter them intraoperatively,” says Alexander L. Neuwirth, MD. “Making sure the components are in the right place is absolutely critical in hip replacement surgery to ensure proper postoperative function. You can also measure leg lengths with much more accuracy before you leave the OR. With the traditional posterior approach, the only way to assess leg length was through palpation of the knees and ankles, which is far less precise than using a combination of intraoperative physical exam and the use of fluoroscopic images.”
“The use of fluoroscopic-guidance imaging during surgery is a boon in evaluating bone preparation, achieving better intraoperative assessment of cup placement, and accurately measuring leg length within millimeters,” says Dr. Geller. “The surgeon can leave the operating room with the confidence that the components are perfectly aligned and sized, thus ensuring a better outcome.”
“Having the patient supine on the operating table facilitates the use of intraoperative fluoroscopy," says Thomas R. Hickernell, MD. "This enables us to position the implants exactly where we planned.”
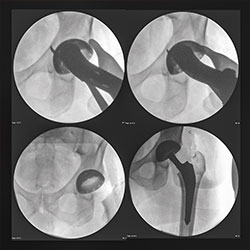
Intraoperative fluoroscopy: assessing acetabular component positioning
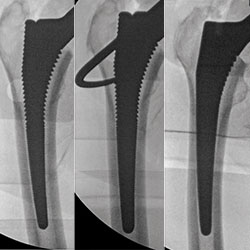
Intraoperative fluoroscopy: optimizing femoral sizing and filling of the femoral canal
The surgeons at Columbia have performed the anterior approach for many years with excellent outcomes. “Our perioperative protocols are aimed at reducing complications, including the use of special dressings for patients who are obese or diabetic and more likely to develop wound healing problems,” says Dr. Cooper. “And our femoral complication rate or risk of fracture is essentially zero percent because we have found that certain stem designs worked better from the anterior approach.”
“We are very attuned to implant shape and design and matching the morphology of the implant with the specific anatomy and bone type of individual patients,” says Dr. Shah. “For osteoporotic bone that is at a higher risk of fracture, this might mean using bone cement, which is somewhat of a dying art in other parts of this country. Our main goal is to give patients a perfect reconstruction. This is the best way to ensure patients get-up-and-go faster, with less pain and less time away from their busy lives.”
Improving Pain Management
In a recent study published in the Journal of Arthroplasty, members of the Columbia arthroplasty team, in collaboration with the Department of Anesthesiology, showed in a cohort of 550 total joint patients that those given preemptive opioids immediately before surgery experienced more pain, consumed more postoperative opioids, and exhibited impaired early function as compared to those who were not given preemptive opioids. Differences in pain and function were more pronounced in patients undergoing total hip arthroplasty than those undergoing total knee arthroplasty.
“We also have streamlined our perioperative care protocol, both with spinal anesthesia and the use of blocks and preoperative pain control,” adds Dr. Cooper. “Our patients require minimal narcotics postoperatively, a significant change from only eight years ago when I was in training.”
“In addition,” notes Dr. Geller, “we are working with anesthesiologists to minimize the effects of anesthesia so that patients ambulate more quickly after surgery.” Adds Dr. Shah, “This is how we can send so many total hip and knee patients directly home a couple hours after surgery.”
“We are always trying to do more to improve pain control and early postoperative function, while reducing the use of opioids, which historically have been the mainstay of pain control in orthopedics in general,” says Dr. Hickernell. “The anterior approach is gaining in popularity because patients have read about it and they care that their recovery is going to be much easier and faster than with the posterior or lateral approach.”
“Patients request the procedure because they know that their friends who have had it are out of the hospital on the same day or next day as opposed to being hospitalized for a few days,” says Dr. Tatka. “They’re back to doing their activities within weeks instead of months.”
“Some 1,000 anterior hip replacements are performed each year at Columbia. Our high volume and experience bring important value to our patients.”
— Dr. Roshan P. Shah



