Quality & Patient Safety Initiatives
Systems-Based Approach to Quality and Safety in Orthopedic Care
Three years ago, the Department of Orthopedics at NewYork-Presbyterian/Columbia incorporated a quality and safety focus as a mainstay of the department’s overall vision and strategy with the appointment of Michael G. Vitale, MD, MPH, as Chief Quality Officer and now Vice Chief of Quality and Strategy.
Under the leadership of William N. Levine, MD, Orthopedic Surgeon-in-Chief, and Dr. Vitale, the department has developed an organizational infrastructure that is transforming orthopedic healthcare delivery. The improvements are driven by a multidisciplinary approach to improving quality, safety, value, satisfaction, and the overall patient experience across adult and pediatric orthopedic subspecialties. The initiatives focus on a number of universal concerns in orthopedic care, as well as on challenges that are relevant to specific procedures. Their work is based on a number of precepts:
Variability Unexplained variability reflects suboptimal care
Infrastructure A chaotic work environment benefits from infrastructure
Group Better decisions are usually made in groups
Data Using data can move the bell curve
Culture Pivot the culture in order to sustain and scale change
“Our processes always involve using best available evidence, harnessing the power of the group, setting goals, working toward those goals, and making the work visible,” says Dr. Vitale. “This five-step process is the foundation of what’s called lean management, which we have incorporated not only as a quality improvement tool, but also as a management tool for our department.”
Quality & Safety Practices
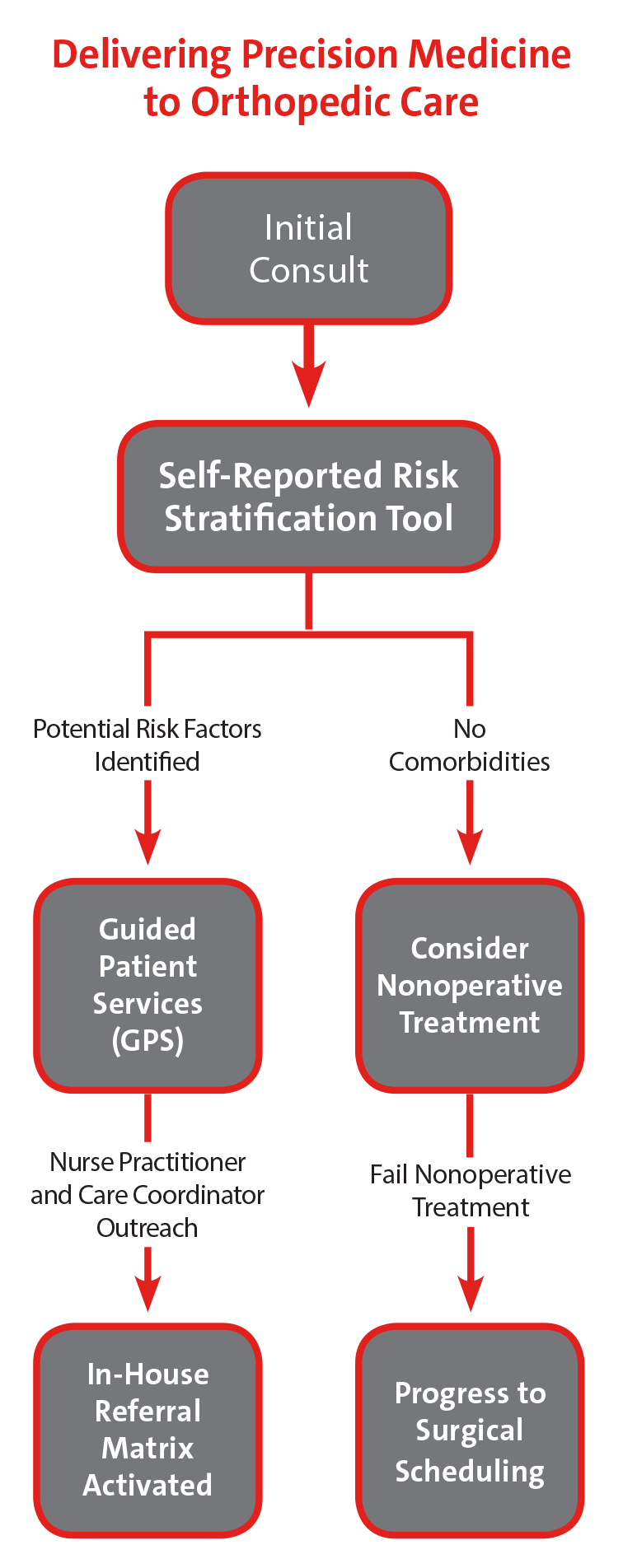
- Risk stratification tools and risk severity scores better identify patients at highest risk for surgical complications
- Surgeon specific dashboards detail performance for select quality, safety, value, and satisfaction metrics drilled down to the origin of the safety issue to define actionable data
- Comprehensive Unit-Based Safety Program (CUSP) AHRQ-funded multicenter program improves patient safety and staff satisfaction through team building and leadership engagement
Comprehensive Unit-Based Safety Program (CUSP): A Case in Point
The Department of Orthopedics uses the CUSP model to build a culture of teamwork across disciplines and inclusive of physicians, nurses, and other clinical team members with a goal of improving processes in a number of areas. Following is one example of CUSP in action.
CUSP Goal
Perform two spine cases in one day The spine team set a goal of performing two spine surgeries in patients with adolescent idiopathic scoliosis in one day by 5 pm. The objective was to reduce the total time from the first-case scheduled start to the time the second case wheels out by 20%. A complementary goal was set to increase staff satisfaction by 25%.
Action Plan
After conducting staff interviews and observations, the CUSP team identified and implemented the following opportunities for improvement:
Quick Wins
- Installed whiteboards in the OR
- Working with vendors, OR nurses and scrub techs reduced the number of trays and instruments needed per case by one-third, decreasing the time allocated to opening instrument packs
- Scheduled nurses on the team to arrive earlier
Metrics
- Adopted a mechanism to track causes of delay
- Tracked time spent in each phase of the OR using swimlanes with timestamps
Results
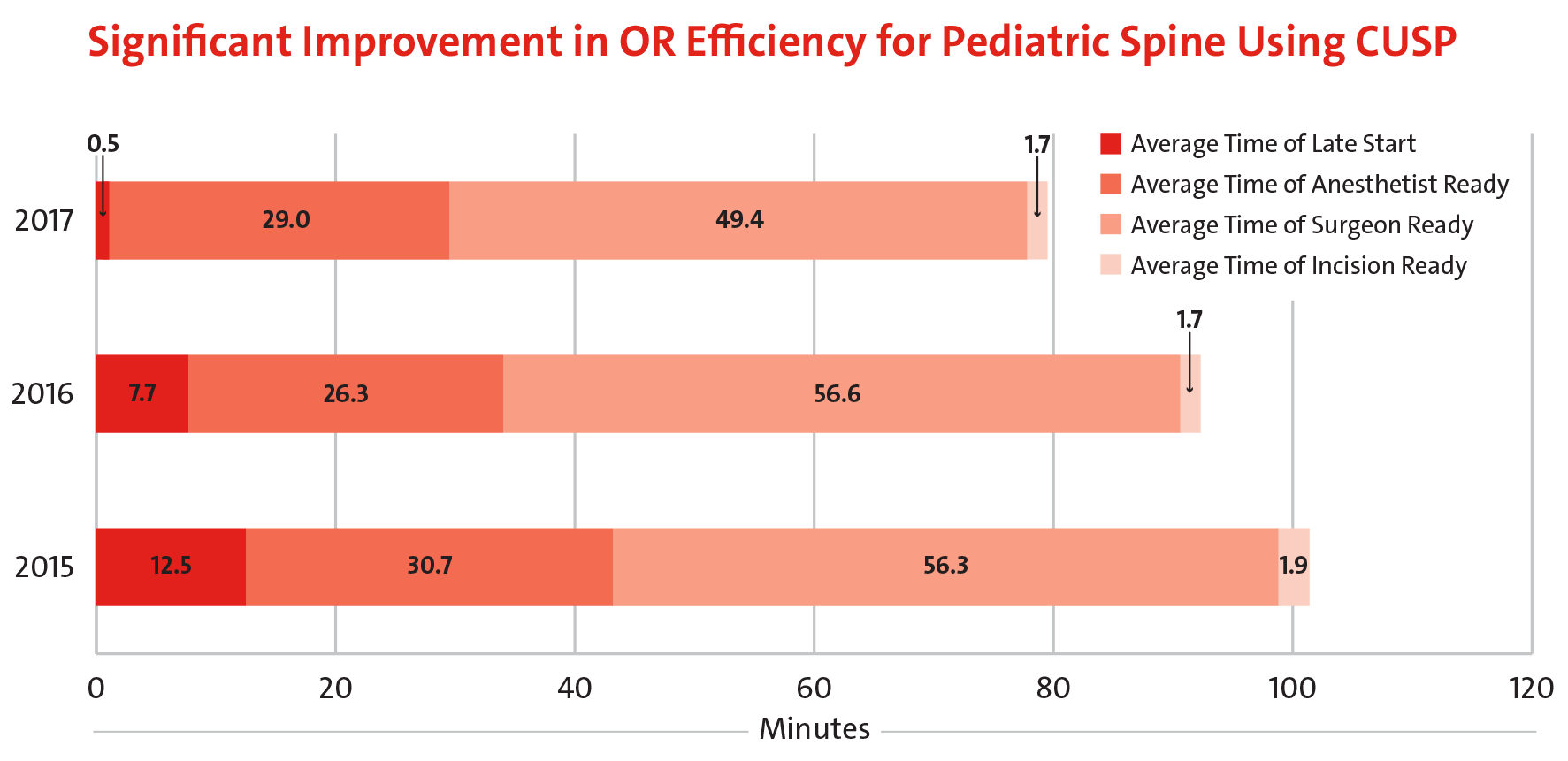
- Average time of late start was reduced by 96% over a two-year period, with a current average of less than one minute.
- Total time to making the incision was reduced by 21% from 102 minutes in 2015 to 81 minutes in 2017
- 35% improvement in OR efficiency versus 2015
An Alternative Application of the Mortality and Morbidity Conference
Applying CUSP
enabled the Department of Orthopedics to increase OR efficiency for adolescent idiopathic scoliosis surgery in 2016 by 35% versus 2015.
In the reorganization of the quality infrastructure for the department, an opportunity materialized to use the monthly Mortality and Morbidity (M&M) conferences of each orthopedic service as a vehicle for department-wide adoption of new practices.
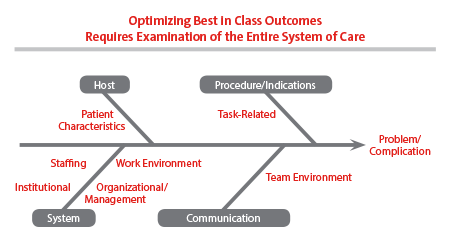
"Medical error is rarely the result of a single, sharp-edge problem and much more often a result of a combination of host, systems, culture, and technique issues,” says Dr. Vitale. “Our M&M conferences are now presented in that structured light. In other words, we use a fishbone process where every suboptimal result or situation that occurs in the department is looked at with a lens of what we could have done differently from the point of view of systems, optimization of host, culture, and technique. When you do this you truly realize how complex the healthcare system is, but it also reveals the many opportunities for improving care that go far beyond the intervention and extend to the entire episode of care.”
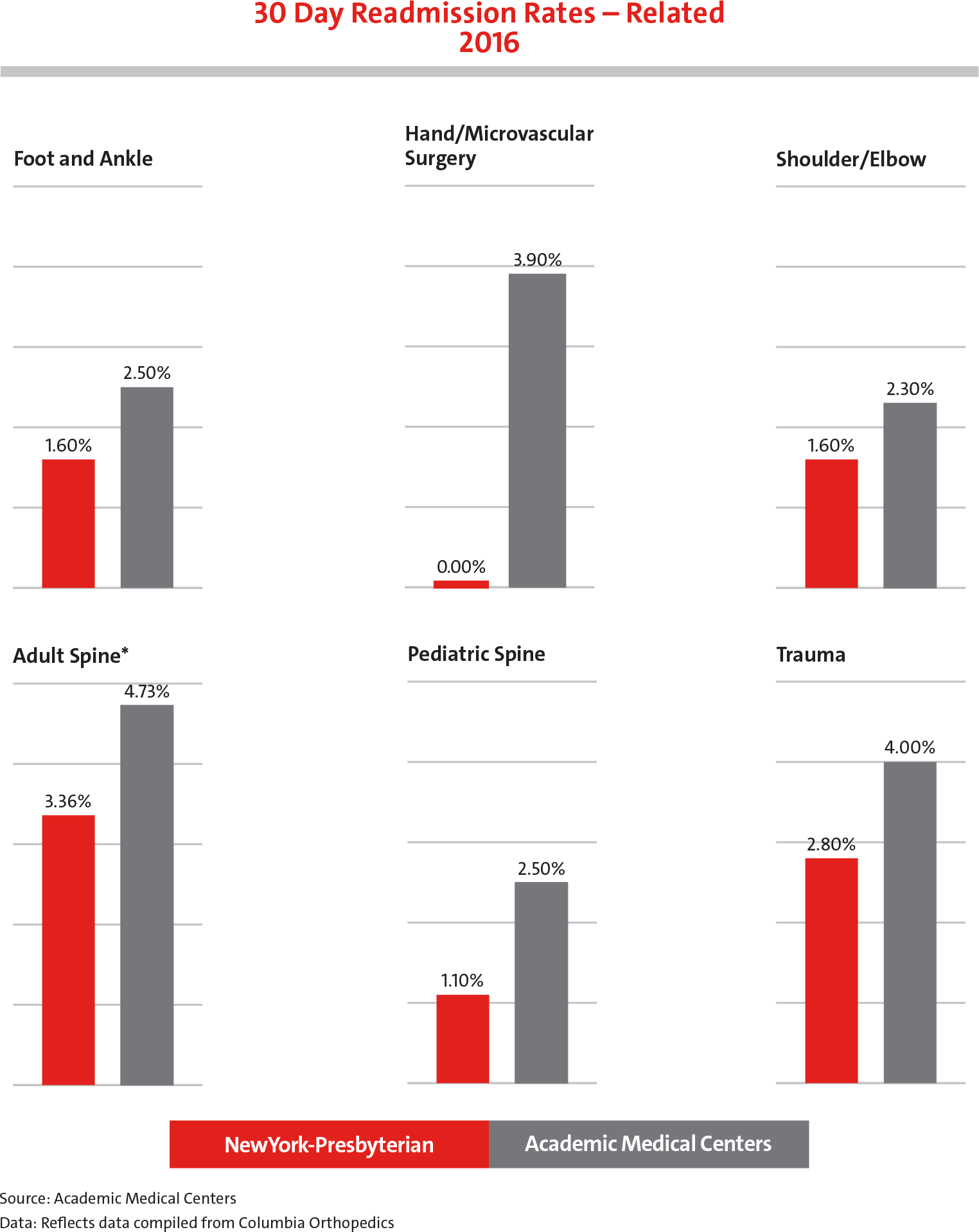
30-Day readmission rates
for every orthopedic service at NewYork-Presbyterian/Columbia are below the national average.
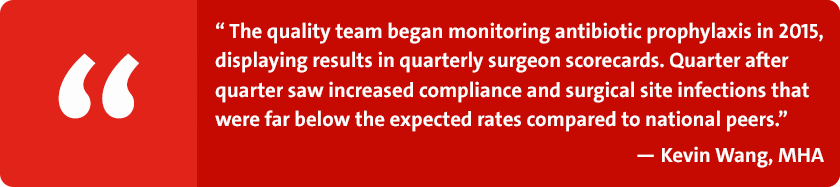
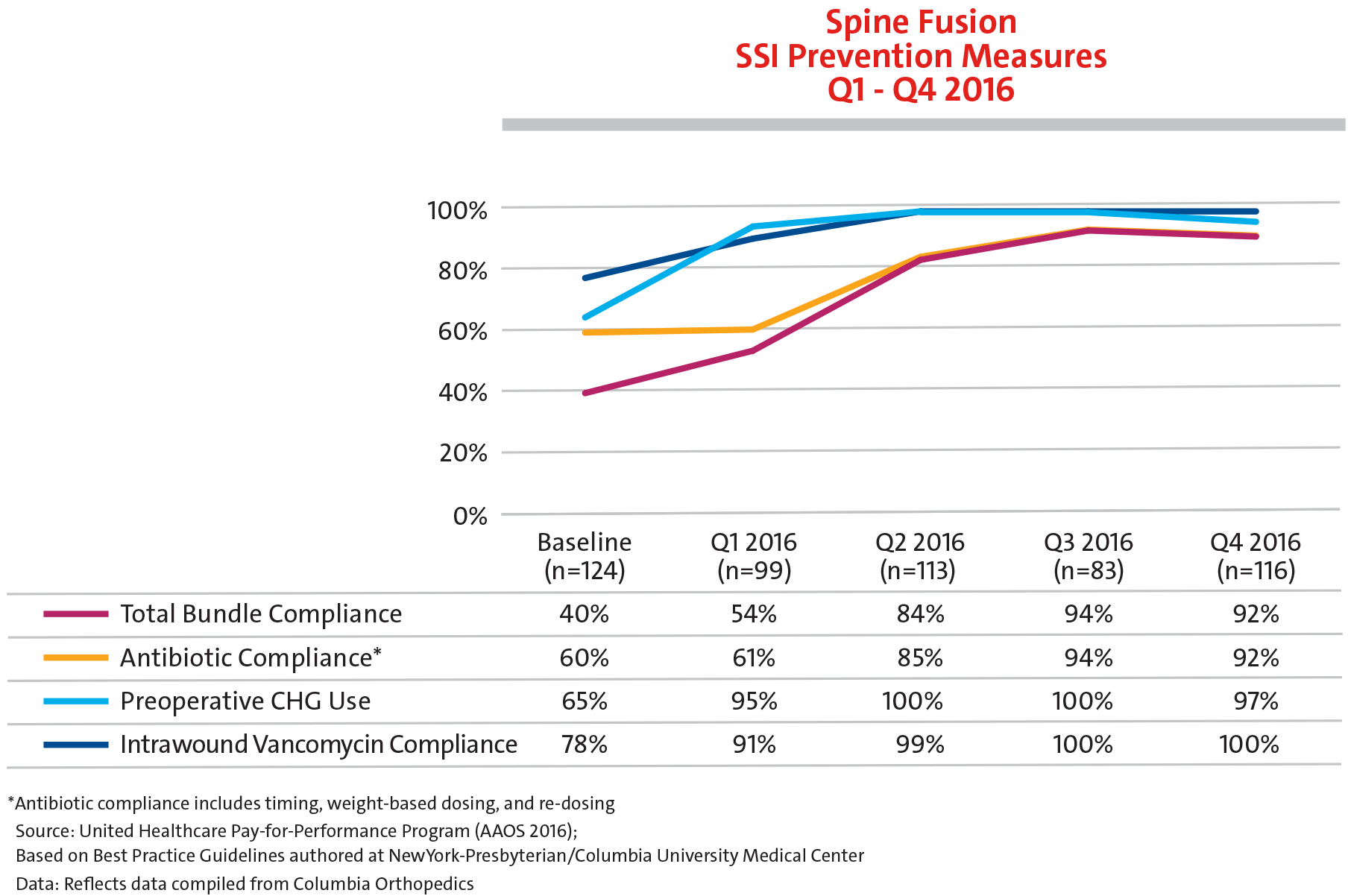
Meeting the Challenges of SSIs
Kevin Wang, MHA
Director, Quality and Value

Safety in Spine Surgery
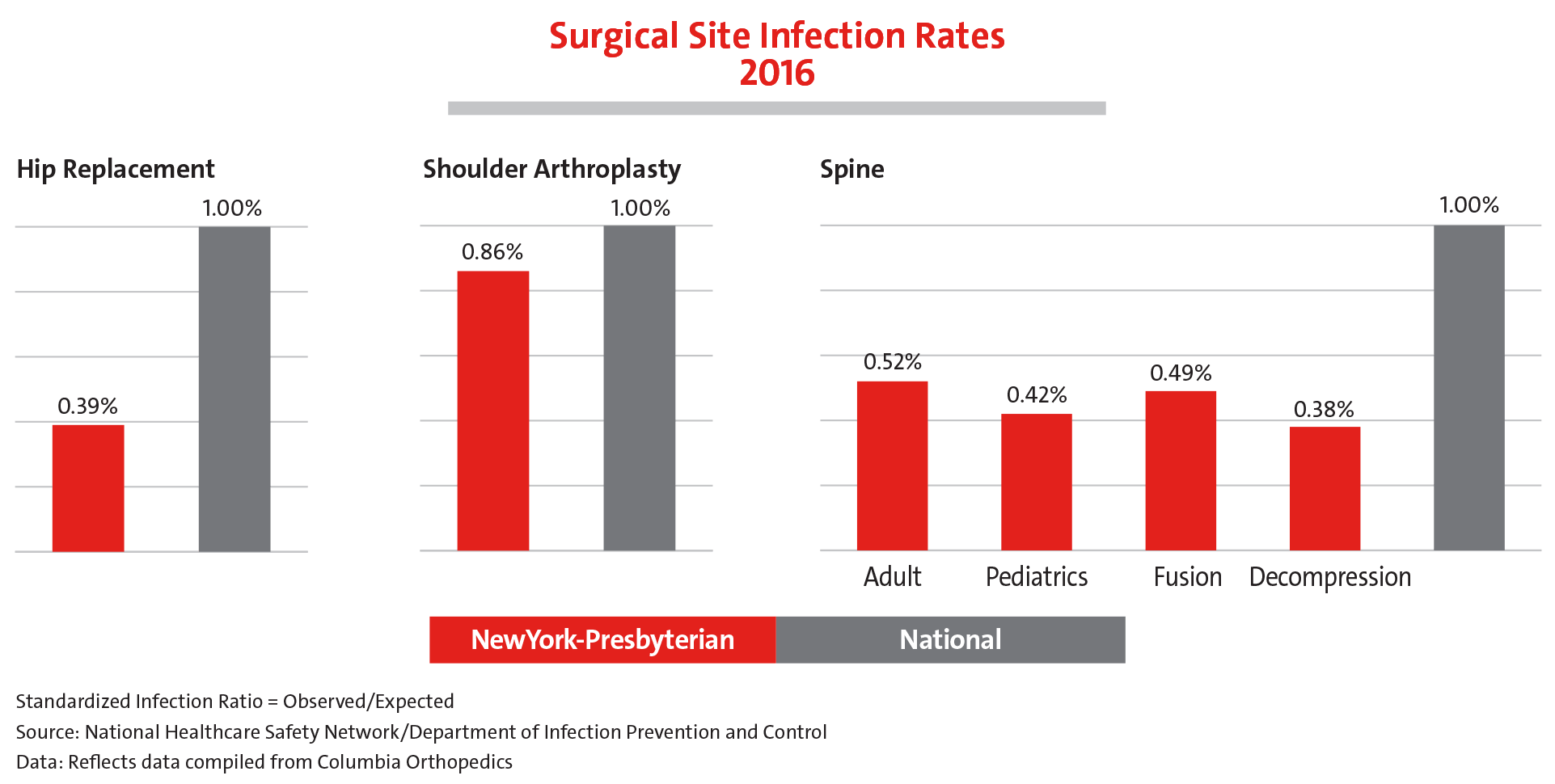
We are proud to report that the surgical site infection rates of Columbia Orthopedics are far below expected rates compared to national peers.
The nature of spine surgery presents surgeons with its own set of challenges. A number of initiatives are underway at NewYork-Presbyterian to address some of the most pressing issues. These include:
- Dual surgeon approach for high-risk spine cases
- Dedicated intraoperative spine team checklist that details required steps from the preoperative stage to pre-incision, to post-incision and pre-instrumentation, to postinstrumentation
- Reviewing postoperative orders with the spine dedicated ICU team
In addition, our surgeons continue to develop best practices:
Preventing Wrong Level Spine Deformity Surgery
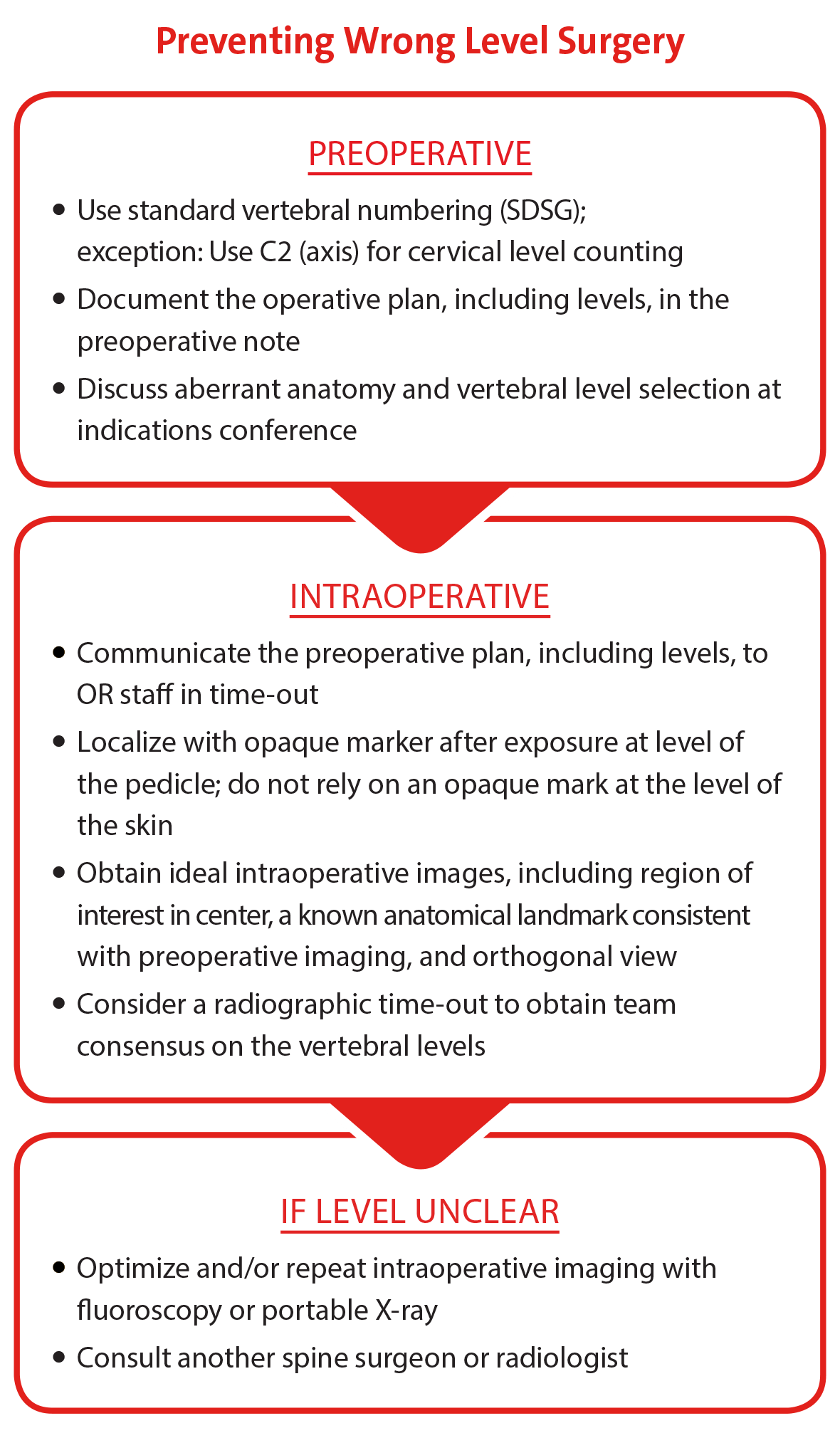
Our spine surgeons have introduced a checklist representing a consensus on items to review before and during surgery in order to confirm the correct vertebral level.
Reducing Deep Vein Thrombosis and Pulmonary Embolism
The establishment of a multidisciplinary team charged with developing best practices for reducing incidence of deep vein thrombosis and pulmonary embolism has facilitated data assessment and brought wide visibility to and incorporation of the team’s goals and efforts. This, in turn, has led to major improvements in quality metrics related to these complications.
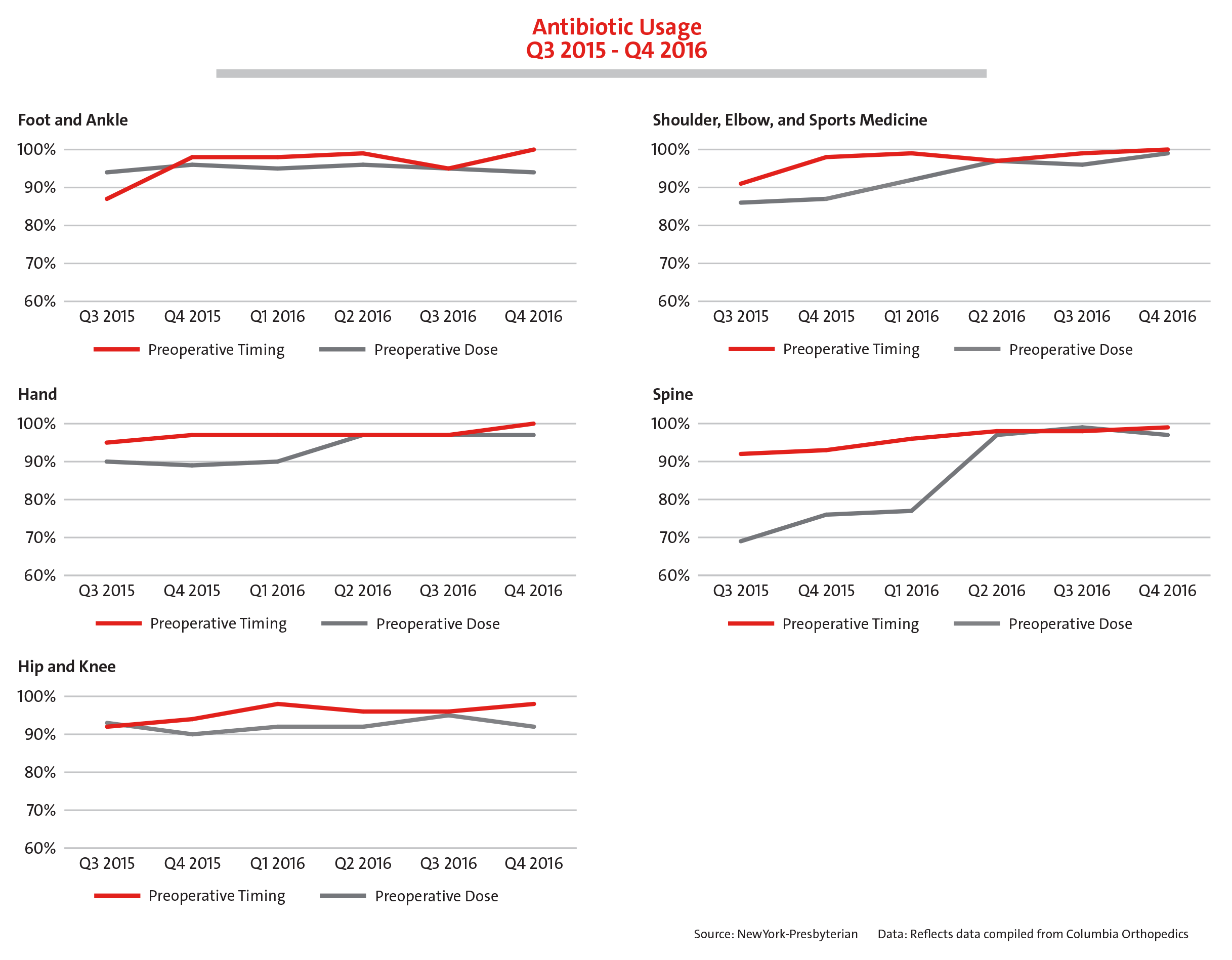
Making Surgical Site Infection a Never Event
Preventing one single infection has dramatic effects on the patients, their morbidity, quality of life, and family unit. But it also has dramatic effects on healthcare costs. With an aspirational goal to have zero infections, our spine specialists have accomplished tremendous foundational work in this area through the implementation of:
- Preoperative bathing regimen
- Standardized protocols for preoperative and intraoperative antibiotic timing and dosing
- Requirement of new, clean scrubs for each spine case
- Terminal cleaning of ORs
Averting Neurological Problems
Employing checklists for responding to intraoperative neuromonitoring changes in patients with a stable spine in the OR prevents major complications from occurring.
Leading the National Conversation
Our spine surgeons are lead authors on a number of peer-reviewed journal articles presenting transformative recommendations for improving safety practices in spine deformity surgery.

Dr. Michael G. Vitale
Vice Chief, Quality and Strategy
In addition to his work at NewYork-Presbyterian, Dr. Michael Vitale plays a major role in advancing the national agenda on quality and safety in orthopedic care. He leads the research arm of the Pediatric Orthopaedic Society of North America’s Committee on Quality, Safety, and Value and is the Vice President of the Board of Directors for the Children’s Spine Foundation, where he also has a leadership role in the Foundation’s Children’s Spine Study Group.
Preventing SSIs in EOS Surgery
Dr. Vitale was a member of a focus group from two multicenter pediatric spine deformity study groups, which developed best practice guidelines for the prevention of SSIs in early onset scoliosis surgery. The guidelines were published in the October 23, 2017, online issue of the Journal of Pediatric Orthopaedics.
The Team Approach
At NewYork-Presbyterian/Columbia, a large pediatric orthopedic case volume has made possible the development of dedicated teams, for example, a pediatric anesthesia spine team and a pediatric spine ICU that are among the only, if not the only, such specialized teams in the country. In addition, approximately one in four pediatric spine procedures is performed with a pediatric spine neurosurgeon. “Our experience shows that with the most complex cases, having two fully trained surgeons, especially one with a somewhat different experience and perspective, really makes a difference,” says Dr. Vitale, who along with his colleagues was invited to author an article entitled, “The Team Approach: How to Achieve Best Outcomes in Pediatric Spine Surgery,” for The Journal of Bone and Joint Surgery.
Safety in Spine Surgery Summit

In 2014, Dr. Vitale founded the Safety in Spine Surgery Summit, which has become one of the most soughtafter conferences in the field, providing an opportunity for leaders from all over the world to come together and talk about best practices. Most recently, Dr. Vitale has set up the S3P – Safety in Spine Surgery Project (safetyinspinesurgery.com), which is linked to the Safety in Spine Surgery Summit, so that continuing education and sharing of best practices in spine care can take place throughout the year.
In February 2017, New-York Presbyterian hosted the 2nd Annual Safety in Spine Surgery Summit for 200 spine surgeons, spine team members, and patient safety leaders from around the country who came together to discuss the numerous safety and quality advances being made in spine surgery for adults and children. The program emphasized that surgical expertise must be combined with strict protocols to minimize complications and to maximize safety. The course agenda was framed around two questions: How will the next patient be harmed? How far will you go to avoid it?
On April 20, 2018, the 3rd Annual Safety in Spine Surgery Summit will be held in New York City.
The theme of the program is "Toward New Rules of Engagement for an Increasingly Complex Spine World” and features a keynote lecture on “Team of Teams” by General Stanley A. McChrystal, a four-star general and one-of-a-kind commander with a remarkable record of achievement. General McChrystal is widely praised for revolutionizing the way military agencies interact and operate. He will share his field-tested leadership lessons, stressing a uniquely inclusive model that focuses on building teams capable of relentlessly pursuing results.