Advances in Research
Dr. Stavros Thomopoulos
Vice Chair, Basic Research
The Department of Orthopedics at Columbia provides an environment in which clinician-scientists and basic scientists collaborate closely with orthopedic surgeons on multidisciplinary musculoskeletal research endeavors, facilitating the link between modern science and clinical care.
Tissue Regeneration: The Holy Grail of Healing
Stavros Thomopoulos, PhD, Vice Chair of Basic Research in the Department of Orthopedics, and Director of the Dr. Robert E. Carroll and Jane Chace Carroll Laboratories for Orthopedic Surgery, is a leader in regenerative medicine. Funded by several NIH R01 grants and an NIH U01 grant, Dr. Thomopoulos and his colleagues are pursuing biologic solutions to solve the challenge of attaching tendon to bone with a particular focus on the most relevant clinical challenge – rotator cuff repair in the shoulder.
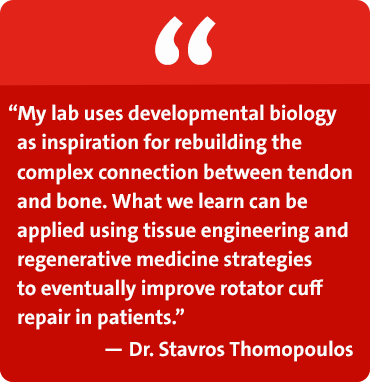
Tendon attaches to bone across a specialized tissue called the enthesis. Over the last few decades, with the design of new suturing methods and devices, surgical repair can now create a secure connection of tendon back to bone. However, mechanical fixation is imperfect in the long term due to a scar-mediated response that fails to recreate the structure and composition of the healthy enthesis. Ultimate success lies in biological solutions that regenerate the enthesis to its pre-injury state and maintain this structure through local cell activity.
Dr. Thomopoulos’ lab focuses on combining the basic building blocks for regeneration of tissue – a cellular component, signaling factors, and scaffolding. A number of studies are underway examining the developmental biology of the enthesis in order to learn how to drive the regenerative process. Their approach identifies stem cells and growth factors critical for fetal and postnatal development of the enthesis and applies them to repair using tissue engineering approaches.
A Unique Population of Stem Cells
Using genetically modified mouse models, Dr. Thomopoulos and his researchers have discovered a particular population of stem cells necessary for building the complex transitional tissue between tendon and bone. By implanting these cells in animal models of tendon-tobone repair, they are seeking to determine if those unique stem cells – when introduced in an adult healing attachment – will be able to regenerate tissue and provide a solution to the challenge of rotator cuff repair.
The Right Signal
The formation of a functional tendon-to-bone attachment requires biologic cues. The researchers are exploring a number of growth factors that stimulate cells, with a particular focus on the signaling factors that promote mineralization and facilitate the formation of a connection between tendon and bone.
A Scaffold for Support
In order to move closer to translation of these research ideas into clinical practice, Dr. Thomopoulos and his team are collaborating with biomaterials expert Helen H. Lu, PhD, a Columbia bioengineer, and William N. Levine, MD, Orthopedic Surgeon-in-Chief, who have been collaborating to create complex scaffolding materials specifically for tendon-to-bone repair. Together, the three professors are now pursuing developmentally inspired solutions for enhanced tendon-to-bone repair. Their effort combines the scaffolds developed by Dr. Lu and her team with stem cells and growth factors identified by Dr. Thomopoulos and his team in order to drive the regeneration of a healthy enthesis.
Intervertebral Disc Degeneration: A Precision Medicine Treatment Paradigm
Dr. Nadeen O. Chahine
Associate Professor of Bioengineering in Orthopedic Surgery and Biomedical Engineering
Nadeen O. Chahine, PhD, Associate Professor of Bioengineering in Orthopedic Surgery and Biomedical Engineering at Columbia University Irving Medical Center, pursues research to understand how biomechanics and mechanobiology of cells and tissues cause a healthy spine to degenerate. Dr. Chahine seeks to understand the variability in the response of patients to treatment and what is present in the patient’s circulation that is contributing to the disease state. Her goal is to identify biomarkers that stratify patients for treatment – medical or surgical – that will lead to better efficacy and outcomes for those patients.
The Inflammation Hypothesis
A major focus of Dr. Chahine’s basic research is on the hypothesis that inflammation is a driving force of spinal disc degeneration and associated pain propagation. Her studies have shown that adult patients who have disc disease also have systemic inflammation. Dr. Chahine believes there are consequences of inflammation that are detrimental to mechanical functions of the disc and therefore need to be addressed at the cellular and molecular level.
Predictive Biomarkers
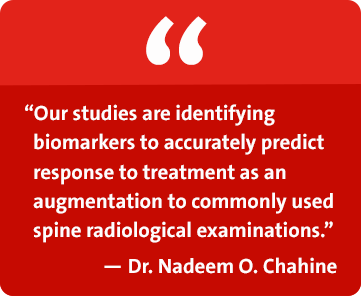
In collaboration with spine surgeons and rehabilitation medicine specialists at the Och Spine Hospital located at NewYork-Presbyterian Allen Hospital, Dr. Chahine is studying the potential for developing a predictive biomarker of pain and response to treatment. They are looking at patients with lumbar disc herniation whose treatments ranged from epidural steroid injections to surgery. The researchers are evaluating patient reported outcome measures, including severity of pain and level of disability, and modeling this information with levels of biomarkers measured in blood specimens preand post-treatment. Based on changes in specific profiles of inflammatory mediators, they are seeking to determine which factors are predictive of change in outcomes. Patients who move on to surgery will continue in the study and all patients will be followed longitudinally up to one year.
Inflammatory Profiles
Dr. Chahine notes that by analyzing inflammatory biomarkers and phenotyping patients based on inflammation, they have already learned that the inflammatory profiles are very different in different kinds of spine conditions. For example, patients who have spinal stenosis and degenerative disc disease have a far higher inflammatory burden in their blood systemically compared to patients who have, for example, disc herniation. And all of the patients with low back pain have inflammatory levels that are far worse than a controlled cohort of patients with no history of back pain.



