Breakthrough Innovations & Interventions
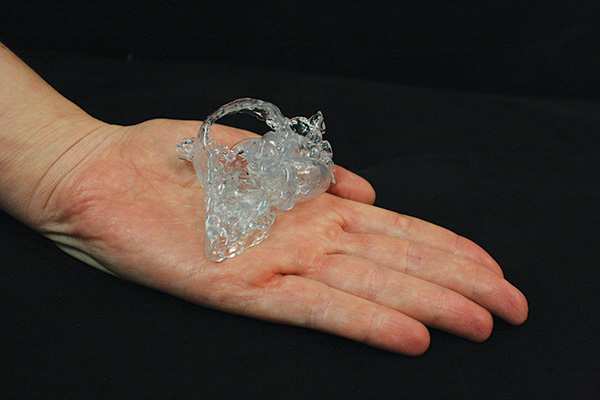
Thanks to this 3-D heart model, cardiac surgeons at NewYork-Presbyterian Congenital Heart Center could plan an infant’s operation before stepping into the OR.
As one of the nation’s leading academic medical centers, NewYork-Presbyterian/Columbia University Medical Center has one of the largest clinical research programs in the country. Our patients have access to still-emerging innovative interventions performed in few hospitals, as well as national studies that improve survival and neurological outcomes for babies.
Our physicians and scientists continue to make groundbreaking contributions to newborn care with procedures and therapies for a range of challenging diseases and disorders.
Notable Achievements Include...
NewYork-Presbyterian physician-scientists are engaged in medical and surgical innovation that has changed the way newborn care is delivered throughout the world.
-
Columbia physician Virginia Apgar developed the now ubiquitous APGAR score in 1952, a simple rapid method for assessing newborn vitality immediately after birth to determine if any medical intervention is required. This method reduced infant mortality and laid the foundation for modern-day neonatology. The APGAR score is still considered the best predictor of infant health in the first month of life and is used throughout the world.
-
In 1984, we performed the first successful pediatric heart transplant in the United States.
-
We were the first hospital to introduce amniocentesis and pioneer its use in detecting birth defects.
-
We founded New York City’s first in vitro fertilization program.
-
NewYork-Presbyterian Morgan Stanley Children’s Hospital pioneered the use of Bubble CPAP or Continuous Positive Airway Pressure for newborns with respiratory distress syndrome. With Bubble CPAP therapy, pressurized oxygen is delivered through the baby’s nose, allowing continuous lung inflation. Babies breathe with assistance as opposed to a machine breathing for them. This low-tech therapy is performed minutes following birth to prevent chronic lung disease. The neonatal intensive care unit at NewYork-Presbyterian Morgan Stanley Children’s Hospital is a recognized leader in this gentle, noninvasive technique and has one of the lowest chronic lung disease incidence rates in the world.
-
In 2014, a team of surgeons at NewYork-Presbyterian Morgan Stanley Children’s Hospital saved the life of a two-week-old newborn using a 3-D printed model of the child’s heart as a guide for surgery on the child, who was born with complex heart defects, including many holes and malformations. With the aid of the 3-D model, the team was able to repair all of the heart’s defects in a single procedure. Typically, babies born with this complex form of congenital heart disease require a series of three or four life-threatening surgeries.
-
In 2014, we successfully delivered a baby whose mother was on a Left Ventricular Assist Device (LVAD).



