Download the Full Report View the E-booklet
Read more about our top research and key innovations from 2025:
A Decade Of Results On Nivolumab And Ipilimumab For Advanced Melanoma
Novel Drug Regimen Shows Promise In Early-Stage Breast Cancer
Trial Using Liquid Biopsy Shows Novel Drug Slows Progression Of Advanced ER+/HER2- Breast Cancer
Dedicated Ophthalmic Oncology Expertise Expands Care Options For Patients
Deep Learning Helps Predict Treatment Response In Muscle-Invasive Bladder Cancer
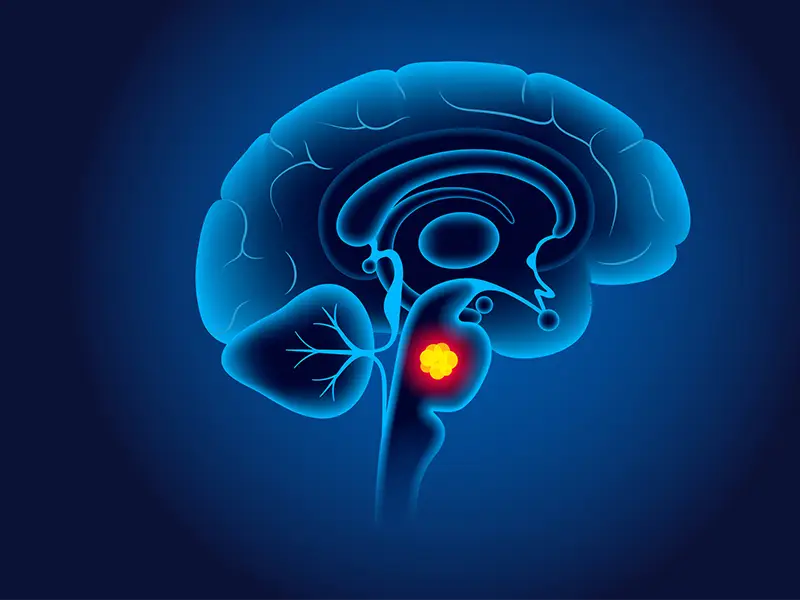
Novel Treatment Method Can Address Aggressive Pediatric Brain Tumor
New Trial Device Opens Blood-Brain Barrier To Treat Glioblastoma
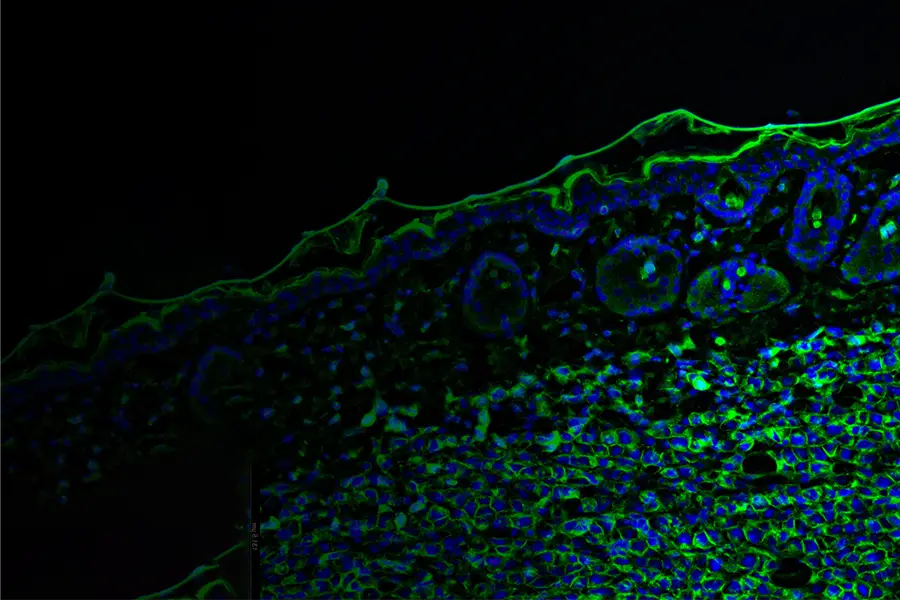
Biomarker Predicts Response To BCMA Car T-Cell Therapy In Multiple Myeloma
Single-Cell Sequencing Uncovers Insights Into Rise In Early-Onset Colon Cancer