A recent study reveals that patients with advanced breast cancer who developed a mutation in the ESR1 gene, as detected through liquid biopsy, and made a proactive switch to a next-generation medication had better progression-free survival than those who stayed on the standard treatment.
This key finding is from the international SERENA-6 trial, a phase 3, randomized, double-blind clinical trial that took place at medical centers across Europe, Asia, and the U.S., including at NewYork-Presbyterian/Weill Cornell Medical Center, NewYork-Presbyterian Queens, and NewYork-Presbyterian Brooklyn Methodist Hospital. The trial focused on patients with metastatic estrogen receptor-positive, human epidermal growth factor receptor 2-negative (ER+/HER2−) breast cancer who switched to camizestrant, a new selective estrogen receptor degrader (SERD). Results from the study were published in the New England Journal of Medicine and presented concurrently at the annual meeting of the American Society of Clinical Oncology.
“These results highlight the value of liquid biopsy in identifying ESR1 mutations before clinical progression occurs, and they demonstrate the potential of SERDs,” says Massimo Cristofanilli, M.D., an oncologist at NewYork-Presbyterian and Weill Cornell Medicine and a member of the SERENA-6 steering committee and coauthor of the paper. “If we can intervene when the tumor burden is lower, we improve our chances of a good outcome for these patients.”
Addressing Treatment Resistance
The current standard of treatment for ER+/HER2− advanced breast cancer is an aromatase inhibitor plus a CDK4/6 inhibitor. The combination blocks the production of ER-stimulating estrogen hormones and inhibits tumor growth, but tumors can recur because they develop ESR1 mutations that keep estrogen receptors active even when estrogen levels are low or absent.
Approximately 40% of ER+/HER2- patients on traditional treatment develop an ESR1 mutation by the time of disease progression, and those mutations are resistant to aromatase inhibitors. Next-generation SERDs, however, work via a different mechanism, binding to and promoting the degradation of the estrogen receptor, a pathway effective against ESR1-mutated cancers.
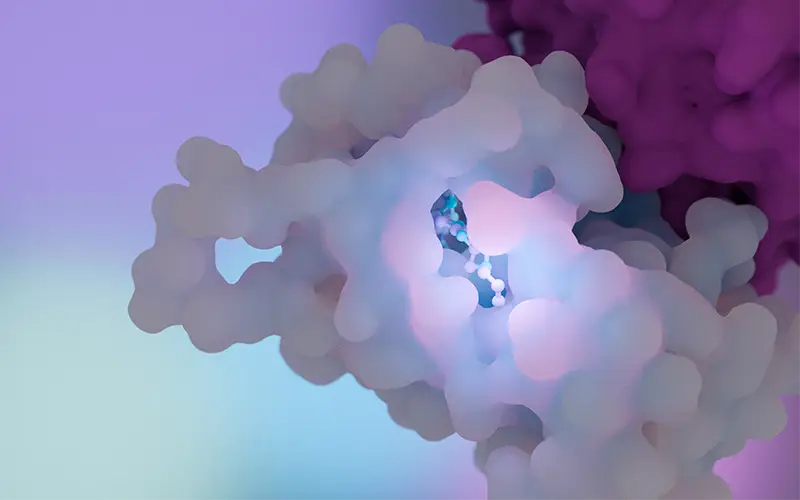
Illustration of camizestrant, a selective estrogen receptor degrader shown to be effective against ESR1 mutations.
“The treatment of ER+/HER2- metastatic breast cancer is based on modulation of the estrogen receptor expression. For many years, our only treatment option to achieve this was endocrine therapy, but we knew that some of these tumors acquired mutational resistance,” says Dr. Cristofanilli, who is also a professor of medicine at Weill Cornell Medicine. “About a decade ago, the first studies of SERDs demonstrated that the combination of one of these agents with a CDK4/6 inhibitor was associated with significant improvement in outcomes like progression-free survival.”
The SERENA-6 study design included both a surveillance period for ESR1 mutations and a double-blind randomization period. More than 3,300 patients were screened at 264 clinical sites in 23 countries. Participants were screened for ESR1 mutations using liquid biopsy technology that measured circulating tumor DNA (ctDNA) every two to three months coinciding with tumor imaging.
“During the surveillance period, if we detected the mutation, we staged the patient, checked if they had a radiological recurrence of disease, and if there was no progression, they were randomized,” says Dr. Cristofanilli.
Three hundred and fifteen patients who had detectable ESR1 mutations with no disease progression were randomized 1:1 into two treatment groups, one that switched to camizestrant and one that continued with an aromatase inhibitor (letrozole or anastrozole). Both groups continued to receive treatment with a CDK4/6 inhibitor (palbociclib, abemaciclib, or ribociclib).
Our results clearly indicate that if we address this mutation before waiting for disease progression on imaging, we can significantly delay progression.
— Dr. Massimo Cristofanilli
The Results
The findings showed that the camizestrant group achieved greater progression-free survival when compared to the aromatase inhibitor group. At the year follow-up, median progression-free survival was 16 months in the camizestrant group versus 9.2 months in the aromatase inhibitor group. At two years, nearly 30% of patients in the camizestrant group were alive without progression, compared to 5.4% in the aromatase inhibitor group.
Quality of life was also measured using patient-reported outcomes. The median time from randomization until a deterioration in self-reported quality of life was 23 months in the camizestrant group and 6.4 months in the aromatase inhibitor group.
“Our results clearly indicate that if we address this mutation before waiting for disease progression on imaging, we can significantly delay progression for these patients,” says Dr. Cristofanilli.
The SERENA-6 study results support the first-line use of camizestrant in patients with an ESR1 mutation. It also exemplifies the usefulness of liquid biopsy to aid in real-time treatment decision-making, something that Dr. Cristofanilli has been working on for over two decades. “By monitoring ctDNA, we can adapt our treatment approach and have a major impact on patients’ quality of life and the overall delay of more aggressive treatment,” says Dr. Cristofanilli.
He notes that additional analyses are planned using the SERENA-6 data, including examining long-term outcomes for patients without an ESR1 mutation. “There is so much that we are going to learn with longer follow-up from the amount of data that we have,” he says. “I think this is going to be a very valuable resource for future studies as well.”




