Download the Full Report View the E-booklet
Read more about our top research and key innovations from 2025:
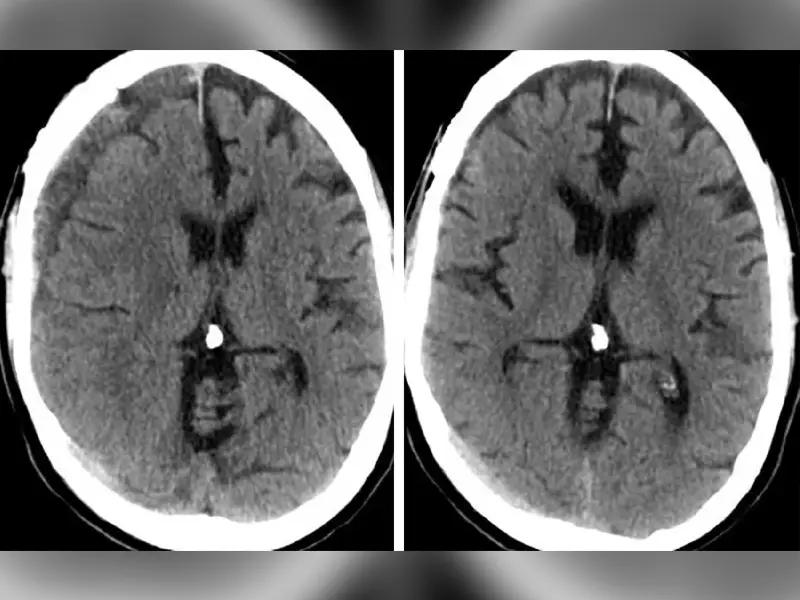
NEJM Study Highlights MMA Embolization Effectiveness For Subdural Hematomas
MVD: The Promise Of Long-Term Pain Relief For Trigeminal Neuralgia
Upright PET Scanner Will Advance Early Alzheimer’s Detection
Experimental Gene Therapy May Treat Aggressive Form Of ALS
Novel Treatment Method Can Address Aggressive Pediatric Brain Tumor
Sleep Spindles Could Be An Indicator Of Hidden Consciousness
Advancing Lasting Biological Solutions for Degenerative Disc Disease
Awake Spine Surgery Designed For Anesthesia-Intolerant Patients
New Trial Device Opens Blood-Brain Barrier To Treat Glioblastoma
Detecting Parkinson’s Disease Sooner with Biomarker Research