Physicians and researchers at NewYork-Presbyterian and Columbia have spent years working to understand the phenomenon of cognitive motor dissociation (CMD), also known as hidden consciousness. Patients with hidden consciousness due to a brain injury appear unresponsive while in a coma or vegetative state, but have brain activation to motor commands similar to conscious patients, according to Jan Claassen, M.D., FNCS, chief of critical care and hospitalist neurology at NewYork-Presbyterian and Columbia.
Current testing to find these traces of consciousness are technically challenging but having that information may carry prognostic significance for long-term clinical recovery. In a new study recently published in Nature Medicine, Dr. Claassen, senior author of the paper, and his colleagues show how certain sleep patterns in unresponsive patients may help predict which patients have CMD, and therefore a better chance of regaining consciousness and eventual function.
“I want to be able to provide more guidance and assurance of what’s going to happen in the future to the loved ones of the patients that I see,” says Dr. Claassen. “When someone is in this acute state with a head injury, when they are unconscious and in the ICU, it can be hard to predict their chance of recovery. If, in that early stage, we can detect awareness, we may be able to give more guidance on what to expect in the next few months or years.”
A Focus on Sleep
In 2019 and 2022, Dr. Claassen and his team published a series of papers in the New England Journal of Medicine and Lancet Neurology demonstrating how they could detect willful brain activation by apply machine learning algorithms to EEG recorded while patients were presented with simple commands, such as to open and close their hand. This systematic brain activation, or CMD, would indicate some residual level of consciousness, which could influence a family’s choices about care and treatment. Unfortunately, those tests can be difficult to implement and may yield unreliable results.
The very same structures in the brain that are involved in maintaining consciousness, however, are also thought to be relevant for sleep. “There is no one spot in the brain that is purely associated with consciousness. There are regions in the deeper structures of the brain and cortex, where if there are injuries, a person’s consciousness is impaired,” he says. “These same regions are also important for controlling and maintaining sleep.”
If we can better understand the reason a person’s consciousness is impaired, we can personalize the treatment for that patient.
— Dr. Jan Claassen
When there is activity within these deeper brain structures, EEG recordings will pick up specific patterns called sleep spindles, which are brief bursts of brainwave activity that occur during non-rapid eye movement sleep, a restful phase of sleep that is crucial for physical and mental recovery and is characterized by slow-wave brain activity, slowed breathing and heart rate, and relaxation of muscles. The study found that detection of these sleep spindles was often a predictor of recovery of consciousness when the patient underwent more sophisticated testing for CMD.
Study Results
Among the 226 unresponsive patients who were monitored for this study, approximately one-third showed evidence of sleep spindles, including about half of patients with CMD, further suggesting an association between the brain architecture that maintains sleep and consciousness. While sleep spindles weren’t a perfect predictor of hidden consciousness — several patients without sleep spindles did recover consciousness — over two-thirds of those with sleep spindles and CMD showed evidence of consciousness by the time they were discharged from the hospital, and over 40% regained neurological function within a year.
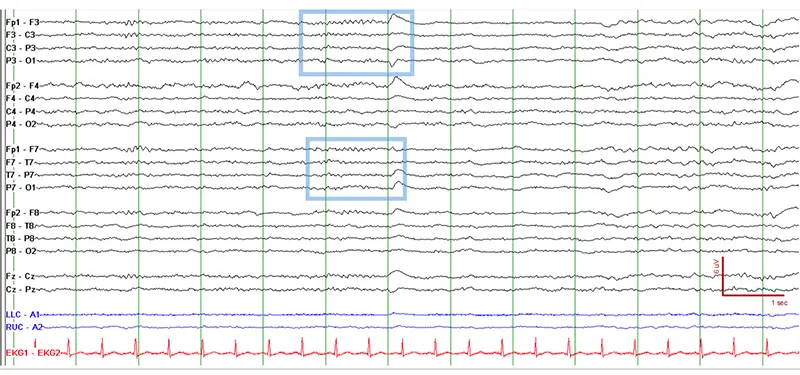
EEG of a comatose patient showing well-formed sleep spindles, pictured in the light-blue box.
“Acute brain injuries are a common problem in the U.S. and beyond,” says Dr. Claassen. “If we can better understand the reason a person’s consciousness is impaired, we can personalize the treatment for that patient. But first we need to determine consciousness, and new tools like identifying sleep spindles will help guide us in our decision-making when we are trying to determine the treatment and outlook for the future of a patient and their overall chance of recovery.”
We’ve shown that you can use a passive activity like sleep to help predict which unresponsive patients will have a better chance at recovery.
— Dr. Jan Claassen
Implications for the Future
Dr. Claassen and his team went through all the EEG recordings by hand to identify the sleep spindles. While there are computer programs that can detect sleep patterns, they are not typically trained on the severely abnormal EEGs of unconscious patients. Feeding this information into a large electronic database could help automate the process in the future, so that machine learning can help detect sleep spindles and allow greater application of this method in other ICUs or neuro rehabilitation facilities.
Dr. Claassen also says they will continue to look for other methods of capturing potential consciousness in patients, such as using smell or sound to elicit a response instead of relying on speech comprehension.
“We want to cast a wide net,” says Dr. Claassen. “We’ve shown that you can use a passive activity like sleep to help predict which unresponsive patients will have a better chance at recovery. This is an exciting moment, and we continue to look for new ways to build on our work and expand our understanding of hidden consciousness. Importantly, we are striving to utilize these novel tools to develop targeted treatments to actively support the recovery of our patients at NewYork-Presbyterian.”