The 2022 Innovations in Review of clinical and scientific advances in oncology highlight NewYork-Presbyterian’s pioneering strategies for early detection and for accelerating the development of personalized therapeutics to achieve the best possible outcomes for our cancer patients. Physicians, scientists, staff, and trainees at Columbia's NCI-designated Herbert Irving Comprehensive Cancer Center (HICCC) and the Weill Cornell Medicine Meyer Cancer Center are at the frontier of research that is helping to transform care for the most challenging cancers and all communities in New York City and beyond.
New: A Paradigm Shift in Radiation Treatment Planning
How Melanoma Prepares Lymph Nodes for Metastases
Reason for Optimism: Advancing Therapy for Triple-Negative Breast Cancer

New: A Paradigm Shift in Radiation Treatment Planning
Radiation oncologists at NewYork-Presbyterian/Columbia are now bringing the latest technology – radiation therapy using artificial intelligence (AI) - to treat certain cancers. Columbia’s new radiation delivery machine, Ethos, is the first-of-its-kind in the New York metropolitan area and surrounding region that uses AI to efficiently fine-tune a patient’s radiation treatment. This new technology solves a long-standing issue in radiation oncology – the difficulty of adapting treatment to anatomical changes in the patient or the tumor that can occur over time. Ethos also allows radiation oncologists to deliver very focused radiation doses to the tumor while reducing its impact on the surrounding structures, thereby avoiding or reducing side effects.
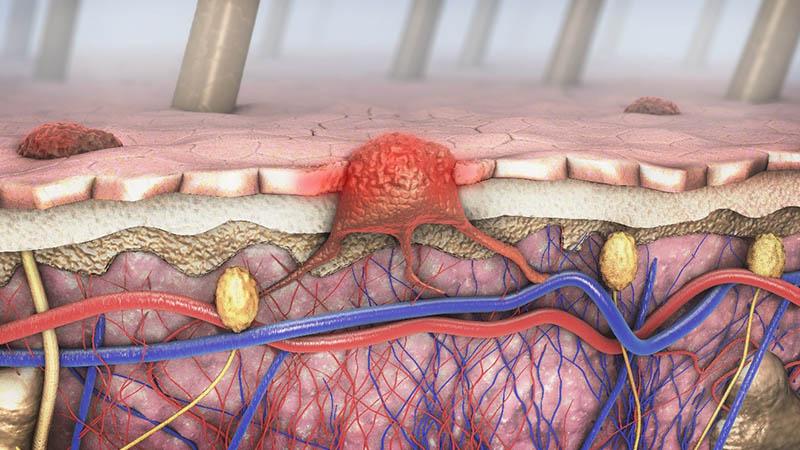
How Melanoma Prepares Lymph Nodes for Metastases
NewYork-Presbyterian/Weill Cornell Medicine clinicians conducted a study that found melanoma cells release small extracellular packages containing the protein nerve growth factor receptor (NGFR), which prepare nearby lymph nodes for tumor metastases. In the findings published in Nature Cancer, the researchers noted that these results may help doctors determine which patients need more aggressive treatment and could help with the development of new targeted therapies.
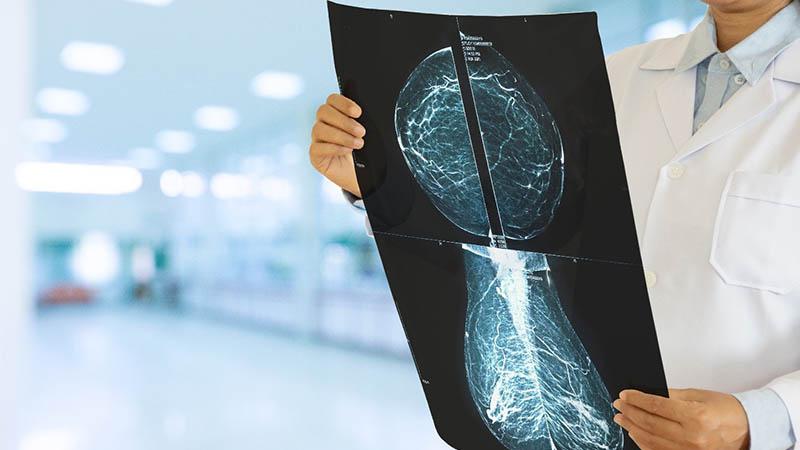
Reason for Optimism: Advancing Therapy for Triple-Negative Breast Cancer
Dawn L. Hershman, MD, MS, FASCO, director of breast oncology and co-leader of population sciences at NewYork-Presbyterian/Columbia, provided her expertise to help develop the American Society of Clinical Oncology (ASCO) Guideline Rapid Recommendation Update on neoadjuvant therapy for breast cancer. Triple-negative breast cancer is an aggressive subtype known for its high recurrence and mortality rates. Following positive results from the KEYNOTE-522 trial in 2021, the FDA approved pembrolizumab, the first immunotherapy agent for early triple-negative breast cancer combined with standard chemotherapy as neoadjuvant treatment for patients. Additional results from the fourth phase of the KEYNOTE-522 trial were published last year, and the updated ASCO guidelines outline dosing recommendations for pembrolizumab as well as guidance around screening and management of adverse events.

Tumor Microenvironment of Lung Cancer: What Lies Beneath?
Through a Cancer Moonshot immunoprevention grant from the National Cancer Institute’s Immuno-Oncology Translational Network, NewYork-Presbyterian/Weill Cornell Medicine doctors are exploring mechanisms that allow slow-growing lung cancer lesions to progress into aggressive malignancies and are working to identify new therapeutic approaches to intercept the transition.
In the first stage of their work, their analysis exposed distinct biologies associated with nodule classifications thereby validating CT density as a clinically actionable diagnostic parameter in the exploration of tumor progression.



