Lung cancer remains the second most common cancer and leading cause of cancer-related deaths in the United States among men and women. Non-small cell lung cancer (NSCLC) accounts for approximately 85 to 90 percent of all lung cancers, with about 2.4 million new cases worldwide and 1.8 million deaths each year.
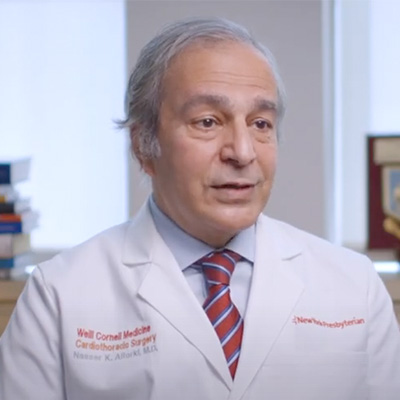
Nasser K. Altorki, MD, is an internationally renowned thoracic surgeon whose commitment to his lung cancer patients is equaled by his passion for furthering understanding of the biological mechanisms of the disease and advancing therapies that can reverse these devastating statistics.
Dr. Nasser Altorki
In his clinical practice, Dr. Altorki, who is Chief of the Division of Thoracic Surgery in the Department of Cardiothoracic Surgery at NewYork-Presbyterian/
In 2019, Weill Cornell Medicine, under the leadership of Dr. Altorki, was awarded a prestigious Cancer Moonshot immunoprevention grant from the National Cancer Institute’s Immuno-Oncology Translational Network to explore the mechanisms that allow slow-growing lung cancer lesions to progress into aggressive malignancies and identify new therapeutic strategies to intercept the transition. In the first phase of the grant, Dr. Altorki and his colleagues have investigated changes in the tumor microenvironment associated with distinct stages of adenocarcinoma – the most common type of NSCLC.
The use of low-dose computed tomography as the standard screening test for lung cancer today has resulted in detection of ground-glass or pure non-solid nodules that could not be seen on plain chest X-rays. “Increased screenings to detect cancer earlier and the development of immunotherapies have been helpful strategies to improve outcomes,” says Dr. Altorki. “But the Holy Grail is to prevent precancerous lesions from progressing to cancer in the first place. An improved understanding of the biology of lung cancer to distinguish normal lung, pre-invasive and invasive nodules is needed to intercept the disease at a clinically meaningful and early point in its progression. Our previous work suggests that the progression from precancerous to aggressive lung cancer is associated with the development of a significantly suppressed immune response in the tumor microenvironment.”
An improved understanding of the biology of lung cancer to distinguish normal lung, pre-invasive and invasive nodules is needed to intercept the disease at a clinically meaningful and early point in its progression.
— Dr. Nasser Altorki
With this in mind, Dr. Altorki and his colleagues in the Department of Cardiothoracic Surgery and the Weill Cornell Medicine Meyer Cancer Center hypothesized that alterations in cells of the tumor microenvironment (TME) have a role in initiating and supporting this progression. Their research focused on CT-detected non-solid nodules, which, according to conventional wisdom, represent pre- or minimally invasive malignancy. But while non-solid nodules are the earliest radiographically detected manifestation of lung cancer, as many as 40 percent of these nodules harbor frankly invasive adenocarcinoma. So, what is causing the transition to more invasive histologies that occur in a significant proportion of these nodules? The answer, note the investigators, lies in understanding the cellular and molecular changes within non-solid nodules and the complex interactions that take place between cancer cells and the surrounding cells, including the immune cells they must suppress to survive.

Non-solid nodule
To accomplish this, the research team analyzed archival tissue samples using whole exome sequencing, global gene-expression profiling, and novel imaging technologies, as well as clinical outcomes data collected from patients treated at NewYork-Presbyterian/
In their current research, the investigators categorized alterations in gene expression and cellular composition of the TME in two groups based on CT scanning: one group with pure non-solid nodules CT density (primarily preinvasive/
Specific findings, published in the April 5, 2022 issue of Cell Reports, include:
- Significant upregulation of genes was involved in remodeling the extracellular matrix (ECM) in pure non-solid (pNS) nodules harboring preinvasive adenocarcinoma and minimally invasive carcinoma
- Expressions of ECM biology genes were further increased in the solid-nodule group, indicating that tumor ECM modification and reorganization continue to evolve over time
- Genes regulating angiogenesis and the broader activation of the adaptive immune response were also enriched in solid nodules compared with pNS nodules, perhaps associated with the continued remodeling of the ECM
- Significant enrichment was found in the expression of chemokine/cytokine genes and their cognate receptors in the pNS-nodule group compared with normal lung; the upregulated chemokine profile was biased toward an immune-suppressive milieu
- Immune TME of the pNS nodules was noteworthy for how few immune-suppressive mechanisms are upregulated in the preinvasive and minimally invasive stages, the principal immune-suppressive mechanism being increased density of regulatory T cells
The authors conclude, “Our data suggest a complex dynamic interaction between the tumor and its immune microenvironment in the very early stages of development…Throughout the entire process, a nascent effector immune response is present but is effectively thwarted by the immune-suppressive elements, suggesting that different interception strategies need to be employed at different stages of tumor evolution.”
“By capturing the cellular and molecular events associated with progression, we can now begin to develop a framework for future studies to develop strategies for early prevention, including immunoprevention,” says Dr. Altorki. The Weill Cornell Medicine researchers are now taking the detailed insights gained in this study on how the composition and activity of the TME changes with progression back to the laboratory. In preclinical studies, they will design and test new therapeutic strategies to intercept lung cancer progression in genetically engineered mice with a more accurate representation of human disease than has been previously possible.