Minimally Invasive or Hybrid Options
Hybrid heart surgery refers to procedures that use conventional surgical methods in conjunction with minimally invasive, catheter-based interventional approaches. Hybrid techniques are performed in a combined procedure with a cardiothoracic surgeon and an interventional cardiologist working side-by-side in the same operating room. These less invasive alternatives use a much smaller incision through the breast bone or right chest, with the advantage of less pain, avoidance of cardiopulmonary bypass, faster return to normal activities and definite cosmetic advantages.
We are one of just a few Centers in the U.S. to have a formal pediatric hybrid program—and the only one in the New York area
Stage 1 Hybrid
At NewYork-Presbyterian Congenital Heart Center, each patient is evaluated for less invasive treatment options first. In some cases, a hybrid approach may enable the team to treat a condition with a single operation rather than a series of surgeries or to treat conditions that would otherwise be inoperable. The Congenital Heart Center is one of just a few U.S. centers to offer hybrid heart operations to infants and children. Our surgeons and interventional cardiologists have extensive experience performing hybrid procedures and we have published many scientific papers on this topic.
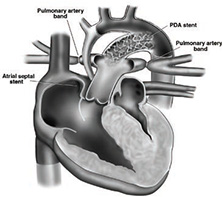
Hybrid Therapy for Hypoplastic Left Heart Syndrome
Center surgeons and interventionalists are successfully using a less invasive hybrid technique for a difficult-to-treat defect in newborns known as hypoplastic left heart syndrome (HLHS). To survive, babies born with this anomaly must undergo surgery in the first week of life. Until recently, the only treatment available was the Norwood procedure, which requires three difficult standard open operations and carries a 10-20% or greater risk of mortality.*
The Stage 1 hybrid procedure removes dependence on the heart-lung machine. At approximately six months, when the baby is better able to handle major open-heart surgery, the second stage operation is performed. The hybrid procedure is thought to be safer in high-risk patients such as low birthweight or premature babies because it avoids use of the heart-lung machine. Hybrid techniques are not applied universally and they are not appropriate for every child. Some babies still do better with the Norwood procedure and we decide on a case-by-case basis, in a multidisciplinary fashion, whether a child will benefit most from one procedure or the other.
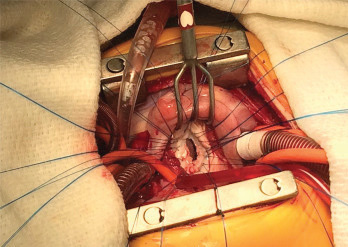
Hybrid Therapy for Ventricular Septal Defect Repairs (VSDs) or Valve Implantation
Center physicians are expanding applications of minimally invasive hybrid techniques to include closing ventricular septal defects or holes in the heart tissue with excellent results.
Typically, holes in the heart are closed by suturing a patch on the hole during open-heart surgery. The hybrid technique allows surgeons to go through the chest and deliver a device to close holes and prevent the need for multiple surgeries. We have developed special instruments that allow us to make these repairs using much smaller incisions than previously possible, resulting in markedly improved cosmetic results.
We have also implanted valves using a hybrid approach, resulting in less need for anticoagulation. Typically, valves are sutured inside the heart and often require anticoagulation with Coumadin. By using stented valves, we can implant biological valves that do not require anticoagulation. Biological valves can also be dilated and enlarged to keep up with the child’s growth, unlike traditional “surgical” valves that cannot be enlarged and must be exchanged surgically.
Sutures are placed around the mitral valve annulus on the atrial side.
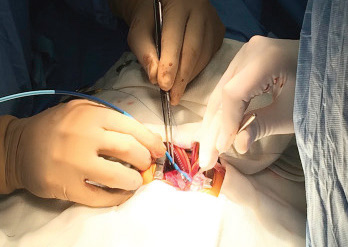
The valve is positioned through the mitral annulus before balloon expansion.
*Source: Society of Thoracic Surgeons Congenital Heart
Surgery Database 2012-2015 Report — mortality for all participating centers: 14.8%



