Early in her pediatric training, Aliva De, MD, knew she wanted to become a pulmonologist, but she couldn’t have predicted that she would be a leader in the diagnosis and treatment of rare lung diseases in children. As Director of the Primary Ciliary Dyskinesia (PCD) Center at NewYork-Presbyterian Morgan Stanley Children’s Hospital and Director of the Pediatric Pulmonology Fellowship Program at NewYork-Presbyterian/Columbia, Dr. De is spearheading efforts to become an accredited Primary Ciliary Dyskinesia Foundation (PCDF) Center.
“The first step in a child's care is an accurate diagnosis. For the longest time PCD was misdiagnosed. It is a rare disease and can have wide range of characteristics,” says Dr. De. “[We] are among the few centers in the New York metropolitan area to noninvasively measure and monitor lung function in children of any age. This testing can provide the critical information needed to choose the most effective treatment and help a child start breathing better as soon as possible.”
Challenges in Diagnosing PCD
Primary ciliary dyskinesia is a rare and progressive genetic disease caused by ciliary dysfunction. Because the clinical features of PCD often overlap with other respiratory diseases, early diagnosis remains a significant challenge for pediatric specialists. Characterized by recurrent and chronic upper and lower respiratory tract infections, pediatric otolaryngologists often receive the bulk of initial referrals. However, families may visit multiple specialists as they struggle to find an accurate diagnosis for their child.
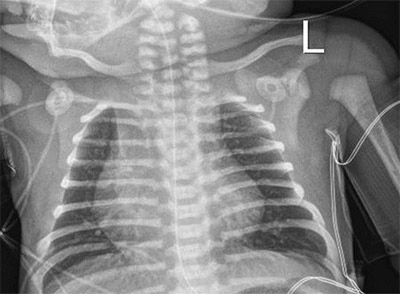
A full-term newborn with respiratory distress and right upper lobe atelectasis should raise suspicion for primary ciliary dyskinesia. This may be associated with congenital heart disease (as in this case with cardiomegaly, also noted on the chest X-ray). (Source: Image courtesy of Aliva De, MD.)
“Sometimes physicians may not have access to all of the tests or understand some of pitfalls and nuances in interpretation of the tests. Phenotypic characteristics in conjunction with positive tests help to establish a diagnosis,” explains Dr. De.
Current estimates suggest mutations in about 50 known cilia-related genes, with more on the horizon as research advances. However, genetic testing is not a definitive diagnosis and must be confirmed with additional tests including:
- Genetic testing
- Nasal nitric oxide test
- Immunofluorescent assay
- Biopsy of ciliary sample tissue
- High-speed videomicroscopy
PCD Clinical Center
NewYork-Presbyterian Morgan Stanley Children’s Hospital is currently in the process of becoming accredited with the PCDF-Clinical and Research Centers Network (CRCN). In order to become accredited, a Center must meet stringent criteria for diagnosing PCD and follow the American Thoracic Society Clinical Practice Guidelines.
The ability to get accredited offers a major advantage. Our Center will be one of the few in the region to provide multidisciplinary care, comprehensive testing, consultation, and treatment for children with PCD.
— Dr. Aliva De
“The nasal nitric oxide test that [NewYork-Presbyterian] purchased is a very useful test. It is very low risk and simple. We can collect longitudinal data, have access to the [PCDF] registry, and provide support and resources to collaborate with other centers,” says Dr. De. “Being part of the PCD patient registry will also allow patients to have access to novel therapeutic trials that are on the horizon.”

The nasal nitric oxide testing device used by the team at the Primary Ciliary Dyskinesia Center at NewYork-Presbyterian Morgan Stanley Children’s Hospital. (Source: Images courtesy of Eco Medics AG.)
Modeled after the success of Cystic Fibrosis Foundation Care Centers, the PCDF plans to grow its network of centers to increase access to high-quality diagnosis and treatment, including groundbreaking research. Nationwide, the PCDF-CRCN currently has about 29 centers in various stages of accreditation.
“There has been a unified effort from the PCD Foundation to have standard guidelines. The more scientific centers we have on this disease will help spread the message and allow patients to have access to comprehensive workup and management,” says Dr. De.
Multidisciplinary Care, Comprehensive Testing
Dr. De’s team at the PCD Center at NewYork-Presbyterian Morgan Stanley Children’s Hospital includes a range of specialists from pediatric pulmonologists to respiratory therapists. Because PCD often involves other organ systems, the team also collaborates with several subspecialists including otorhinolaryngology, neonatology, cardiology, infectious diseases, as well as colleagues in the Adult Center to provide long-term, comprehensive and holistic care services to patients and families.
NewYork-Presbyterian Morgan Stanley Children’s Hospital expects to receive PCDF accreditation in 2023. “The ability to get accredited offers a major advantage. Our Center will be one of the few in the region to provide multidisciplinary care, comprehensive testing, consultation, and treatment for children with PCD,” says Dr. De.



