Total Shoulder Arthroplasty: Guidelines for Discussing Patient Expectations
William N. Levine, MD, Chief of the Orthopedics Service at NewYork-Presbyterian/Columbia University Irving Medical Center, and Chair of the Department of Orthopedic Surgery at Columbia, embraces and advocates a philosophy that engages patients in every aspect of their care. In the operating room and in his department’s laboratories, Dr. Levine displays his internationally renowned clinical skills and research expertise. When talking with patients, he shares yet another side of his professional reputation.
“My clinical practice is predicated on my patients leaving my office with all their questions answered, including a complete understanding of what their treatment options can offer,” says Dr. Levine, who specializes in shoulder, elbow, and knee surgery, and sports medicine.
Charles M. Jobin, MD, Director of Columbia’s Orthopedic Residency Program, and a specialist in shoulder and elbow disorders in adults, concurs. “When patients come to see me, they will have a thorough physical exam and history, but also education about their injury or disease and what to expect afterward.”
Dr. William Levine
Dr. Charles Jobin
When a gap in understanding patient expectations and satisfaction with outcomes following anatomic total shoulder arthroplasty was identified, Dr. Levine and Dr. Jobin undertook a study to align clinical factors with patient perspectives of pain and function. Always seeking to impart their patient-centered convictions to the residents and fellows who seek out Columbia Orthopedics for their training, they included on the study Nathan S. Latham, MD, shoulder and elbow fellow, and Joel R. Peterson, MD, MBA, fourth-year resident, along with Rifa Ahmed, MS, research project administrator.
Research in the literature has shown that formal assessment of outcome measures as reported by patients has become “increasingly relevant to outcomes reporting after shoulder procedures such as a rotator cuff repair and shoulder arthroplasty.” The retrospective case-control study by the Columbia research team involved clinical outcomes data on 67 patients who had undergone anatomic total shoulder arthroplasty between 2017 and 2020, with evaluation at baseline and at a minimum one-year postoperative follow-up. Assessment was performed using the ASES score – a 100-point scale that is weighted 50 percent for pain and 50 percent for function/activities of daily living. The scale includes a physician-rated and patient-rated section with tabulation incorporating both a pain visual analog scale and rating of 10 functional items related to activities of daily living.
To the authors’ knowledge, this was the first study to provide an analysis of anchor-based clinical differences in patients undergoing anatomic total shoulder arthroplasty.
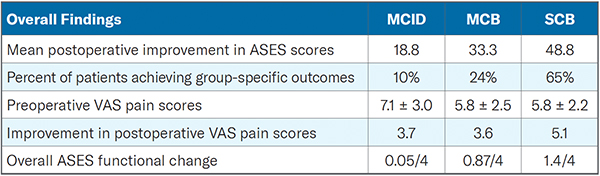
Using prior studies for reference, the Columbia orthopedics study team established three clinical outcome groups with an anchor-based global rating of change assessment to characterize and compare pain and functional outcomes as follows:
- Minimal clinically important difference (MCID)
- Moderate clinical benefit (MCB)
- Substantial clinical benefit (SCB)
At one-year post surgery, patients received a global rating of change anchor assessment comprised of a single question asking them to “compare their overall present condition to their preoperative condition.” Their responses were used to determine clinically meaningful change in outcomes.
The study’s findings, published in the November 19, 2021, issue of the Journal of Shoulder and Elbow Surgery, demonstrated:
- The MCID group had higher preoperative pain scores and the least amount of preoperative functional deficits compared to the MCB and SCB groups
- Outcomes in the MCID group was achieved largely through pain improvement while the MCB and SCB were achieved through meaningful pain and functional improvement
- Patients with higher preoperative pain scores and minimal preoperative functional deficit did not do as well clinically as those patients who had lower preoperative pain scores and greater functional deficits
- Washing, reaching for a shelf, and throwing were the most common functional deficits experienced preoperatively and accounted for the largest improvements in function postoperatively
- Patients with more physical dysfunction realized more benefit from shoulder arthroplasty
- Patients who most benefited from shoulder arthroplasty had the greatest improvement in pain scores
The authors note that information provided from the study can assist orthopedic surgeons in their discussion of possible outcome scenarios with patients considering anatomic total shoulder arthroplasty and facilitate shared decision-making.
Read More
Characterization of ASES score pain and functional improvement after anatomic total shoulder arthroplasty: a patient-centered perspective. Ahmed R, Lanham NS, Peterson JR, Jobin CM, Levine WN. Journal of Shoulder and Elbow Surgery. 2021 Nov 19:S1058-2746(21)00810-7.
Related Publications