Neuroendovascular Interventions: Rescuing and Protecting the Brain from Stroke
Neuroendovascular surgery has undergone a rapid evolution since it first emerged as a specialty, with neuroendovascular therapies for the treatment of both ischemic stroke and intracranial aneurysms showing great promise for improved diagnosis and clinical outcomes.
The neuroendovascular surgeons, interventional neuroradiologists, and neurologists at NewYork-Presbyterian are leaders in performing innovative catheter-based and minimally invasive surgical treatments for complex vascular diseases of the brain. Through endovascular neurosurgery programs at five campuses, patients throughout the region – from Westchester County to Manhattan, Brooklyn, and Queens – benefit from having access to the vast experience and highly specialized skills of these physicians. The following article presents the latest advances in the field taking place throughout the NewYork-Presbyterian system.
Ahead of the Times in Stroke Treatment
Until January 2018, thrombectomy to remove a blood clot in victims of stroke had to be performed within a six-hour window. Results of two major clinical trials showed that some strokes progress more slowly and may still be treatable at least up to 24 hours after onset. This prompted the American Heart Association/American Stroke Association to release new treatment guidelines for acute ischemic stroke patients. Data from clinical trials now support extending the timeframe to 24 hours based on very specific brain imaging, resulting in a far larger world of patients who can benefit from treatment with thrombectomy.
Dr. Sean D. Lavine
“There are individuals whose treatment can extend beyond the 24-hour time window,” says neurosurgeon Sean D. Lavine, MD, Clinical Director of Neuroendovascular Services, NewYork-Presbyterian/Columbia University Irving Medical Center. “If they have enough collateral circulation, other blood vessels in the brain can supply the area of the brain where the artery is occluded. The tissue may be supported just enough to prevent a stroke for quite some time. While there currently are no trial data supporting stroke intervention past 24 hours of being symptom-free, this is an area of investigation that may allow us to help even more patients.”
According to Dr. Lavine, brain imaging has reasserted a central role in the evaluation of stroke patients. “Some individuals, based on genetics and brain blood flow patterns, are eligible for treatment long after the conventional time limit. The decision-making process to treat relies on ‘mismatch imaging.’ We are looking for a mismatch in areas of the brain that have already sustained permanent damage versus other parts of the brain that remain viable but at risk for having a stroke. Patients with this pattern are still able to benefit from treatment.”
Automated CT perfusion imaging in ischemic stroke serves as an important adjunct, along with CT angiography, to conventional unenhanced CT brain imaging, enabling differentiation of salvageable penumbra from the irrevocably damaged infarct core. It has become an essential decision-making tool for thrombectomy versus medical care in acute ischemic stroke because it can identify those patients outside the conventional 4.5-hour window for use of intravenous tissue plasminogen activator (tPA) who have salvageable brain tissue and should undergo a thrombectomy procedure.
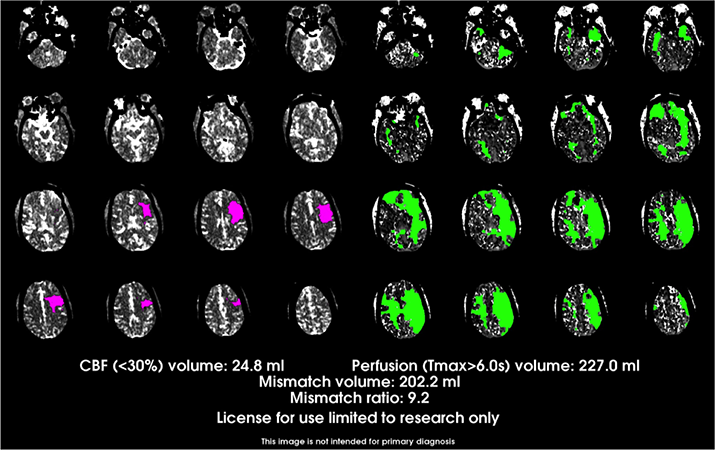
RAPID™ CT perfusion maps help determine if the patient has a perfusion mismatch in comparison to the size of the infarct core. Areas in pink represent brain regions with substantial reductions in cerebral blood flow representing “core infarct;” regions in green represent significant hypoperfusion (reduced blood flow) that is likely still viable brain tissue.
NewYork-Presbyterian neuroendovascular teams use the RAPID™ automated CT perfusion (CTP) software to identify appropriate candidates for thrombectomy. “There are cutoffs for the amount of tissue that can be infarcted in order to do a thrombectomy,” says Dr. Lavine. “If the patient has had a very large stroke and you restore blood flow to that part of the brain it can cause this tissue to hemorrhage and make the situation worse than it actually was. So, the first requirement is that the patient does not have a certain amount of tissue that’s already injured irreversibly. Rapid CTP is the gold standard for identifying the size of the core infarct and deciding how much brain tissue is still salvageable.”
With the benefit of this advanced imaging technology, NewYork-Presbyterian is in a position to offer thrombectomy treatment at five campus sites: NewYork-Presbyterian/Columbia, NewYork-Presbyterian Lawrence Hospital, NewYork-Presbyterian/Weill Cornell, NewYork-Presbyterian Queens, and NewYork-Presbyterian Brooklyn Methodist Hospital.
Dr. Babak Navi
“We’ve participated in several randomized trials that have proven the value of performing endovascular therapy for select stroke patients,” says Babak B. Navi, MD, MS, Division Chief, Stroke and Hospital Neurology, NewYork-Presbyterian/Weill Cornell Medical Center. “The National Institutes of Health DEFUSE 3 trial – of which both Weill Cornell and Columbia were enrolling sites – as well as the DAWN study have shown the benefit of late thrombectomy from 6 to 24 hours post onset of a large vessel occlusive stroke. DEFUSE 3 was a landmark trial. It demonstrated that in patients with a large vessel occlusion identified within six to 16 hours of onset, opening the occlusion through mechanical thrombectomy increases the odds of a good neurological outcome at 3 months by two- to three-fold as opposed to not opening the occlusion.”
“Both trials confirmed that some people have enough blood flow to the areas around the stroke that could still be saved,” says Dr. Lavine. “These trials demonstrated that through either a mismatch between completed stroke on MRI versus the clinical severity of deficits on physical exam, or through CT or MRI perfusion imaging, you can establish that a patient has a large area of the brain tissue at risk for completing to a full stroke. If you intervene and open up the artery before that occurs, you can substantially reduce the odds of serious, long-term disability and even death.”
Dr. Joshua Z. Willey
“While there may be a subset of patients that could benefit from thrombolysis in an extended window beyond four and a half hours, the main study showed a large bulk of those patients were probably eligible for a thrombectomy instead,” says Joshua Z. Willey, MD, MS, Director of Acute Stroke Services at Columbia, which along with Weill Cornell, has been certified by The Joint Commission and American Hospital Association as a Comprehensive Stroke Center. “We have rapid access to perform a thrombectomy. We can get hyperacute MRIs or CTs to determine if the patient has a perfusion mismatch in comparison to the size of the infarct core. If that is present, we use the automated software to determine if that patient is eligible for a thrombectomy.”
“If we’ve identified a large area of salvageable tissue, then we have two options,” continues Dr. Willey, who is board certified in vascular neurology and neurology. “We can offer the patient participation in the trial with tenecteplase, a clot-busting agent that may offer an advantage over the currently available treatment with tPA. Regardless of whether or not they take that clot-busting agent, they are then taken for a thrombectomy.”
Novel Approaches for Stroke Prevention and Treatment
Dr. Grace K. Mandigo
“Technologies are being developed at a rapid pace that provide us with a number of different tools to treat stroke in new ways,” says Grace K. Mandigo, MD, Associate Program Director, Neurological Surgery, NewYork-Presbyterian/Columbia. “Every year we are able to offer interventions with new devices for different subsets of patients who present with acutely debilitating strokes. Virtually any patient with an intracranial aneurysm is a potential candidate for an endovascular treatment and we see very frequently that our interventions make a rapid clinical difference in the outcomes.”
MMA Embolization for Subdural Hematoma
Dr. Jared Knopman
In 2017, Jared Knopman, MD, a neurosurgeon and interventional neuroradiologist in the Weill Cornell Brain and Spine Center, began performing middle meningeal arterial (MMA) embolization for chronic subdural hematoma, the first physician worldwide to implement this approach as a first-line alternative to surgical drainage. “In the past, we’ve treated subdural hematoma through a craniotomy to remove the hematoma and cauterize the membranes to stop the bleeding,” says Dr. Knopman. “A subdural hematoma can encompass half of the skull, and we only open up a small part to drain the blood. Roughly 15 to 20 percent will recur because these membranes continue to ooze in the area that you can’t shut down. In some studies, as high as 33 percent of patients will require retreatment after evacuation.”
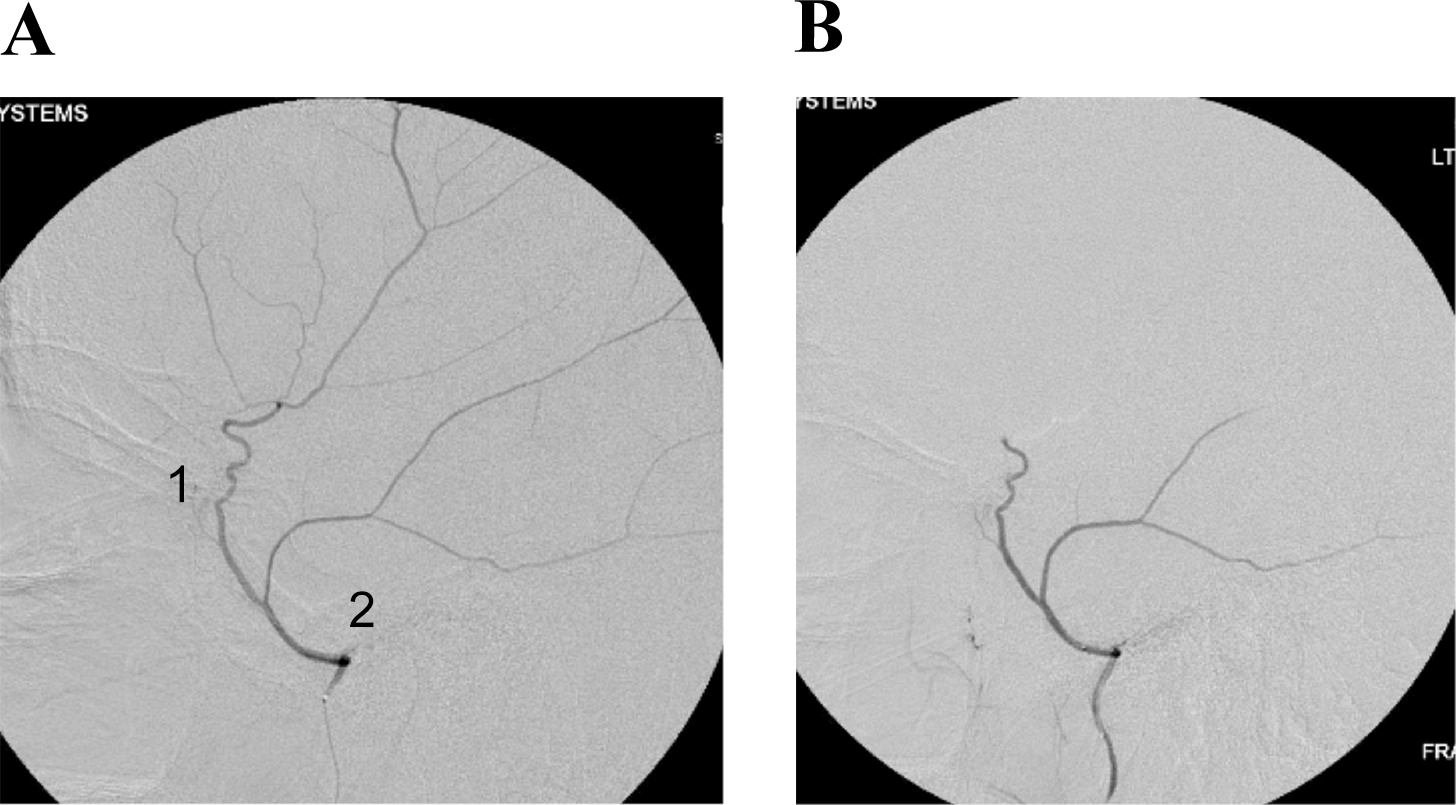
Given the generally advanced age and medical comorbidities of the patient population, Dr. Knopman was committed to finding a minimally invasive treatment to address this common yet complex condition. He developed the groundbreaking technique of MMA embolization using angiography, selective microcatheterization of the MMA, and infusion of polyvinyl alcohol particles. The success of this approach has been nothing short of extraordinary, upending prior medical understanding of subdural hematomas.
(A) Common configuration of the middle meningeal artery with a common trunk that divides into frontoparietal (1) and squamosal/temporal (2) branches. (B) With this configuration, embolization can be performed with the microcatheter tip proximal to the bifurcation of these branches to achieve safe embolization of the maximal amount of dura.
“With embolization of the middle meningeal artery we are able to interrupt the blood supply that keeps these subacute and chronic subdural hematomas alive and that causes them to bleed and rebleed and grow over time,” says Dr. Knopman, who to date has treated more than 300 patients with this approach. “In these 300 plus patients, which represents the largest number of cases in the world, we have had a 92 percent chance of avoiding surgery in patients who traditionally would have met surgical criteria. In patients whose subdural hematomas are too large and require surgery, we have used the modality as an adjunct, which has dropped the recurrence rate from about 20 percent to 3.5 percent. In addition, the complication rate for the procedure is less than one-third of 1 percent – essentially the risk of an angiogram.”
In October 2020, Dr. Knopman began recruiting patients for a randomized clinical trial involving 40 centers in the United States. The trial seeks to enroll more than 500 patients who have undergone surgery for subdural hematomas. “We believe this large sentinel trial will solidify MMA embolization as true standard of care to treat subdural hematoma,” says Dr. Knopman, who serves as Principal Investigator. “We’re going to be testing the recurrence rates with embolization and also looking at patients who have nonsurgical subdurals to see if embolization decreases their risk of needing surgery in the future in that it prevents the subdural from growing. This is going to be the definitive study to establish its acceptance worldwide.”
Flow Diversion for Brain Aneurysms
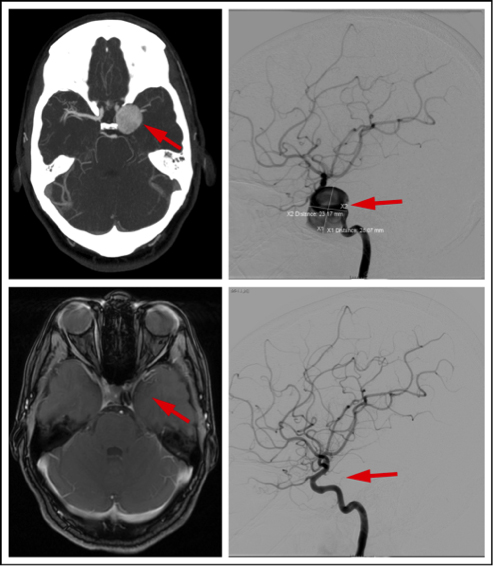
Flow diversion is an endovascular technique whereby instead of placing a device inside the aneurysm sac, such as with coiling, the device is placed in the parent blood artery to divert blood flow away from the aneurysm itself. In properly selected patients, the risk is very low with a cure rate up to 96 percent. Columbia and Weill Cornell neurosurgeons use the Pipeline™ Flex Embolization Device for the treatment of brain aneurysms. Approved by the Food and Drug Administration for the endovascular treatment of adults with large or giant wide-necked intracranial aneurysms in the internal carotid artery, in February 2019 approval was extended for the additional indication of use in the treatment of small or medium-sized intracranial aneurysms. Dr. Knopman’s team has recently published their results using the Pipeline flow diverter for the treatment of aneurysms, demonstrating complications rates in less than 1.5 percent of patients – the lowest quoted complication rate in the literature.
A flow diverter is a stent device that is placed inside a brain artery to treat a cerebral aneurysm. The CT scan points out a giant cerebral aneurysm (arrow, upper left). A cerebral arteriogram provides guidance for minimally invasive treatment of the 28-millimeter aneurysm (arrow, upper right). Treated with a flow-diverting stent, the wall of the artery heals around the flow diverter, and the aneurysm becomes walled off, and then disappears on the MRI scan (arrow, bottom left). A final arteriogram shows complete healing of the artery and no aneurysm (arrow, bottom right).
“Flow diverters are best for treating ‘side-wall’ aneurysms, those that arise from the wall of the artery. Some aneurysms arise where the blood vessel branches, so-called ‘bifurcation’ aneurysms,” says Dr. Lavine. To address this issue, the team at NewYork-Presbyterian has been using the recently approved Woven EndoBridge (WEB®) Aneurysm Embolization System, which enables treatment of aneurysms that occur at a place where the artery is branching in two different ways without the need for a craniotomy to surgically clip the aneurysm. Weill Cornell and Columbia physicians were among the first in the country to use this cutting-edge technology.
Columbia was also a principal site for the multicenter SCENT trial evaluating the Surpass Flow Diverter System – a minimally invasive, single-stent treatment option for patients harboring large or giant wide-neck intracranial aneurysms, particularly large/giant aneurysms arising from the intracranial internal carotid artery up to the ICA terminus. The new system facilitates flow diversion across a wide range of device and blood vessel sizes. Outcomes showed that the Surpass flow diverter successfully occluded intracranial aneurysms without clinically significant parent artery stenosis or the need for retreatment in the majority of patients. This led to the device becoming the first flow diverter to be indicated by the FDA to treat large and giant posterior communicating artery aneurysms.
Following the deployment of flow diverters, dual antiplatelet therapy is typically employed as a means to lessen thromboembolic complications. Dr. Lavine foresees in the near future the development of devices that are coated with an agent that will not require dual antiplatelet therapy. “The next concept beyond that would be devices that may provide a scaffolding for the body to repair an aneurysm, for instance, and then naturally dissolve,” he says. “The patient is not left with any metal or need for antiplatelet drugs or any of the long-term effects of leaving a foreign body behind in the blood vessel.”
Applying Neuroendovascular Procedures for Uncommon Conditions
Over the past two years, neurosurgeon Ning Lin, MD, and interventional neuroradiologist Srikanth Reddy Boddu, MD, MSc, collaborated on the establishment of a multidisciplinary program at NewYork-Presbyterian Queens. The program, which draws on several specialties, including neurology, neurosurgery, emergency room radiology, and the medical ICU, is now operational and capable of providing 24/7 interventional treatment for stroke. Both Dr. Lin and Dr. Boddu apply their specialized expertise to care for patients with unusual presentations.
Moyamoya Disease
Dr. Ning Lin
Dr. Lin has a particular interest in the care of patients with moyamoya disease. “This chronic and progressive condition of the arteries in the brain causes the large blood vessels to become stenotic, leaving the smaller perforating branches to take over delivery of the main blood supply to the brain,” explains Dr. Lin. “Moyamoya means puff of smoke in Japanese. On angiogram, the hypertrophy to perforating vessels forms a smoke-like appearance, giving the disease its name. The narrowing of the blood vessels can lead to blockages resulting in ischemic or hemorrhagic stroke.”
Lateral 3D reconstruction from a CT angiogram of a patient with moyamoya disease.
According to Dr. Lin, direct revascularization involving the superficial temporal artery to middle cerebral artery bypass is the surgical procedure routinely used for adults with moyamoya disease. “When bypass is not technically feasible in adult patients, we will perform cerebral revascularization surgery using pial synangiosis, a method of indirect revascularization initially used only in pediatric patients that has become more widely accepted for use in adults,” notes Dr. Lin, who, in 2014, led a study that supported the use of pial synangiosis in adults. “In patients with a normal arachnoid membrane, dissection with good harvest of the graft is a safe and durable method of cerebral revascularization.”
Pulsatile Tinnitus and Pseudotumor Cerebri
Dr. Srikanth Boddu
Pulsatile tinnitus is characterized by rhythmic whooshing or thumping sounds within the ear that are in sync with a patient’s heartbeat or pulse. “Pulsatile tinnitus affects only a small percentage of the population, and a subset of patients experience it to a debilitating degree,” says Dr. Boddu. “Pulsatile tinnitus may be the only presenting symptom of an underlying serious condition, such as dural arteriovenous fistula, intracranial arteriovenous malformation, venous sinus stenosis, or pseudotumor cerebri.”
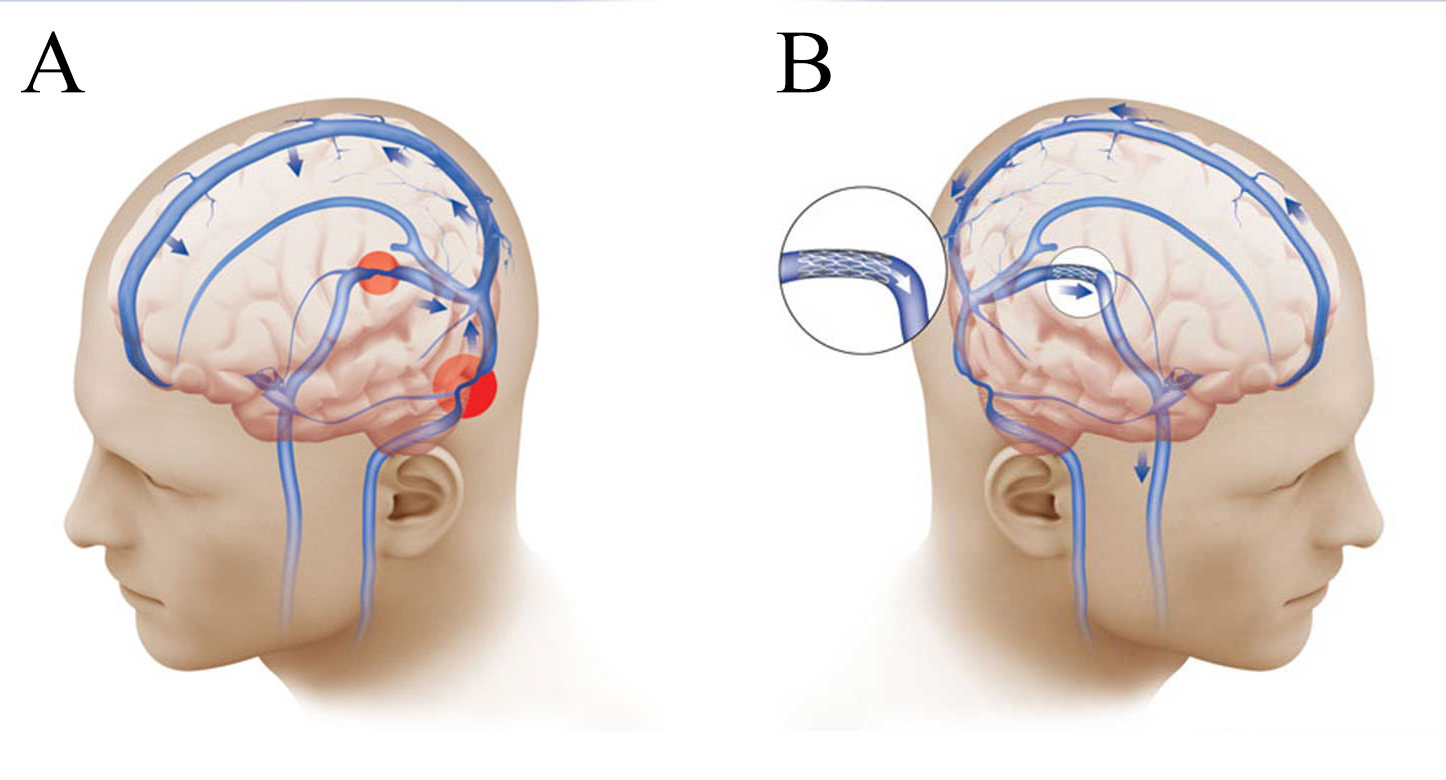
(A) Illustration of bilateral venous sinus narrowing (red circles). (B) Venous sinus narrowing has been treated with placement of a stent, restoring the blood flow from the brain to the neck (blue arrows), and relieving the increased intracranial pressure and the symptoms of pseudotumor cerebri.
Dr. Boddu has particular expertise in venous sinus stenting, a procedure he calls a life-changing option for patients with pulsatile tinnitus who have sought relief for years without success. “There is increasing evidence that venous pathology is causing the overall problem with pulsatile tinnitus and pseudotumor cerebri,” he says. “These disorders have venous sinus stenosis in common. With venous sinus stenting, you can safely widen one of the narrowed veins, restoring good blood flow and eliminating symptoms. Conventional treatment relies on medications, but many people do not respond or cannot tolerate the side effects.”
“Pulsatile tinnitus may be the only presenting symptom of an underlying serious condition, such as dural arteriovenous fistula, intracranial arteriovenous malformation, venous sinus stenosis, or pseudotumor cerebri.” — Dr. Srikanth Boddu
Dr. Boddu is actively enrolling patients in an ongoing venous sinus stenting trial. “We are one of the few centers nationally that is successfully using venous sinus stenting for these conditions on a large scale. Patients who undergo this procedure no longer have the ringing sensation and significant improvement in headaches and vision symptoms.”
Comparing Outcomes: Mobile Stroke Unit vs On-Site ED Care
Weill Cornell and Columbia researchers are now participating in the multicenter BEST-MSU study – BEnefits of Stroke Treatment Delivered Using a Mobile Stroke Unit. The study will help determine whether treatment of stroke via a mobile stroke unit is more clinically effective than treating stroke the traditional way through the emergency department. “This trial has completed patient enrollment and we expect to have the data analyzed and answers to the study questions by early 2021,” says Dr. Navi, site investigator for Weill Cornell. “Hopefully we will have shown that treating acute ischemic stroke with IV tPA in the pre-hospital setting through a mobile stroke unit is a superior strategy and leads to better outcomes. Additionally, if having a patient’s stroke initially diagnosed and classified in the field leads to earlier endovascular therapy, this could also drive better outcomes.”
Endovascular Neurosurgery Across NewYork-Presbyterian
NewYork-Presbyterian/Columbia University Irving Medical Center
NewYork-Presbyterian Lawrence Hospital
Sean D. Lavine, MD
Grace K. Mandigo, MD
NewYork-Presbyterian/Weill Cornell Medical Center
Jared Knopman, MD
NewYork-Presbyterian Brooklyn Methodist Hospital
Michael J. Ayad, MD, PhD
NewYork-Presbyterian Queens
Srikanth Reddy Boddu, MD, MSc
Ning Lin, MD