A Commitment to Conquering ALS
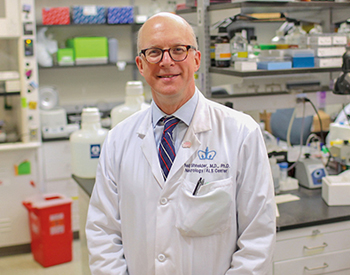
Dr. Neil A. Shneider
Clinicians and scientists at the Eleanor and Lou Gehrig ALS Center in the Department of Neurology at NewYork-Presbyterian/Columbia University Irving Medical Center are leading efforts on a number of fronts to combat amyotrophic lateral sclerosis (ALS) and related forms of motor neuron disease. In addition to providing the latest therapies, they are conducting integrated translational research that ranges from the genetics and basic biology of ALS to the testing of promising therapeutic candidates in clinical trials.
Eleanor and Lou Gehrig ALS Center
Each year, approximately 500 patients with ALS, primary lateral sclerosis, and progressive muscular atrophy come to the Eleanor and Lou Gehrig ALS Center at NewYork-Presbyterian/Columbia.
“Beginning with diagnosis and continuing through each stage of the disease, our subspecialty-trained neurologists and multidisciplinary team members strive to optimize and support the highest possible level of functioning, independence, and quality of life for our patients and their families,” says Neil A. Shneider, MD, PhD, a physician-scientist with expertise in neuromuscular disease and Director of the ALS Center.
“There are well over 25 genes that have been implicated in ALS, and the challenge to the research world is to understand how it is that mutations in so many genes can cause a stereotyped motor neuron disorder like ALS.”
— Dr. Neil A. Shneider
At the same time, Dr. Shneider has engaged basic scientists, cell biologists, molecular biologists, and geneticists to advance the pace of therapeutic discovery in the science of ALS.
“In the last 10 years, we have gained considerable insight into the genetics of ALS, a very complicated disease,” says Dr. Shneider. “There are well over 25 genes that have been implicated in ALS, and the challenge to the research world is to understand how it is that mutations in so many genes can cause a stereotyped motor neuron disorder. What is genetics telling us about pathways and mechanisms of disease shared by all these different forms of ALS? You would think that the genes would all point to a very clear causal mechanism, but they have not.”
In recent years, Dr. Shneider and his colleagues have begun to iterate a unifying theory about ALS. “I think that we are making real progress in our understanding of disease mechanisms that will enable us to take a rational approach to therapy using both traditional and non-traditional approaches.”
With the discovery in late 2011 of the C9orf72 gene mutation as the single most common cause of familial ALS and a related disease, frontotemporal dementia (FTD), Dr. Shneider and his colleagues realized that ALS and FTD are clinically, pathologically, and genetically related and that many of their patients have some degree of frontotemporal dysfunction, if not dementia.
“This provided researchers with a genetic target and, as a result, a great deal of effort is focused on this one form of ALS,” says Dr. Shneider. “For example, antisense oligonucleotides technology used to treat spinal muscular atrophy — a related motor neuron disease — is now being tested in C9-ALS patients in the hope that it will prevent or stop the disease by targeting it at its source. There has been a great amount of success in this arena, which will facilitate its application to other diseases.”
Precision Medicine Sets its Sights on ALS
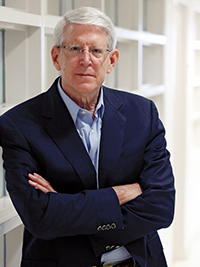
Dr. Tom Maniatis
Tom Maniatis, PhD, is Director of the Columbia Precision Medicine Initiative and a co-founder and currently Scientific Director and Chief Executive Officer of the New York Genome Center, of which Columbia is a partner. Dr. Maniatis, who is also a molecular neuroscientist with Columbia’s Mortimer B. Zuckerman Mind Brain Behavior Institute, pioneered the gene-cloning methods that gave a generation of scientists the tools necessary to identify the genes that cause disease. Today he uses advanced genetics and molecular and cellular biology to identify potential causes of neurological and neurodegenerative diseases, including ALS, which has been a particular focus of his research for nearly 15 years.
“A great deal of effort involving a number of people at Columbia has led to the establishment of initiatives that are directed towards the genetic analysis of ALS and the use of that genetic information to understand its disease mechanisms,” says Dr. Maniatis. “About 10 percent of ALS cases are familial; the remaining 90 percent are sporadic.”
In 2015, Columbia researchers identified a new gene associated with sporadic ALS called TBK1 through a major study co-led by David B. Goldstein, PhD, Director of the Institute for Genomic Medicine at Columbia, involving next-generation genetic sequencing of the exomes of nearly 3,000 patients with sporadic ALS. Subsequently others showed that genetic changes in TBK1 also cause familial ALS. TBK1 is among several “autophagy” pathway genes identified by ALS genetic studies. Thus, this critical cellular pathway has emerged as an “Achilles heel” for ALS disease mechanism studies. A better understanding of how mutations in this pathway cause motor neuron death could lead to finding a cure.
Dr. Maniatis and his colleagues recently reported that autophagy suppresses disease progression early on, but in later stages accelerates the deadly spread of the disease through the spinal cord. Their findings in mouse models, which were recently published in the Proceedings of the National Academy of Sciences, provide a window into ALS’s earliest stages, as well as new insights into its complexity, namely the differing roles that autophagy plays in its progression. In addition, this study can help scientists search for ways to detect and even treat the disease before the onset of devastating symptoms that gradually rob patients of movement, speech, and life.
“One of the biggest barriers to treating ALS is that its progression is dynamic — many different cell types and mechanisms are involved — so treating it at one stage of the disease might have very different, and potentially harmful, consequences at a different stage,” says Dr. Maniatis, the study’s senior author. “Here, we’ve identified a cellular process that likely plays a central role at the very beginnings of the disease, which could open the door to treatments that stop ALS before it has a chance to gain a foothold in motor neurons.” Autophagy is governed by many genes working in concert across every cell in the body, so Dr. Maniatis and his team are now studying how mutations in these genes affect disease progression in an ALS mouse model.

Dr. Matthew B. Harms
Matthew B. Harms, MD, a clinician-scientist in neurophysiology and neuromuscular medicine, directs the ALS Center’s genomics program. “Our relationship with Columbia’s Institute for Genomic Medicine and our proximity to the New York Genome Center have allowed us to make the ALS Center the country’s foremost research resource for ALS and genetics,” says Dr. Harms. “At the ALS Center, we are endeavoring to create the first genomically characterized patient cohort that pairs with Columbia’s precision medicine initiative. Patients who come here have the opportunity to participate in whole-genome sequencing projects. We ask if they are interested in learning the results about known ALS genes if we find a causative mutation and we will provide them with any genomically actionable findings that come out of our research. We don’t know of any other clinic in the country that’s doing this.”
“As we learn more about genotype correlations, we’re hoping to be able to provide information on prognosis based on those genetic findings, and eventually to tailor therapy based on the patient’s genetic profile,” adds Dr. Harms. “If we find someone with a mutation or a set of mutations in a gene that regulates autophagy, then we could use a drug to ramp up or inhibit autophagy depending on the scenario.”
Dr. Harms also leads a multisite effort using whole-genome and transcriptome sequencing to bring precision medicine to ALS. He serves as the Principal Investigator for the ALS Precision Medicine Initiative through the Genomic Translation for ALS Clinical Care (GTAC) project in which researchers are seeking to identify common and distinct features of ALS cases, and to better understand how genes influence the clinical features of the disease. In collaboration with the ALS Association, GTAC involves a combination of next-generation genetic sequencing and detailed clinical phenotyping in 1,500 people with ALS gathered at 10 sites across the country. The goal is to provide a basis for the development of more individually tailored therapies for ALS.
“The GTAC project grew out of the ALS Exome Consortium that Dr. Goldstein and I led in previous years, which was the first study to use whole-exome sequencing to identify a new ALS gene using burden collapsing analysis,” says Dr. Harms. “This technique uses algorithms to identify regions of the genome that are more abnormal in people with the disease than in people without the disease. GTAC will allow us to look for abnormal genes and gene expression profiles that help determine why a person develops ALS and related motor neuron diseases and why their symptoms present and progress with a particular pattern.”
In addition to sequencing the genomes, the researchers are also doing transcriptome profiling, examining the expression level of RNAs in a given cell population. “This gives us a snapshot of the person’s blood cells — what genetic programs are turned on or turned off at that moment,” says Dr. Harms. “We suspect that there will be subgroups of patients, based on those profiles, that will allow us to group people biologically as opposed to clinically. We have to know this if we are going to be able to stratify patients into clinical trials and target autophagy drugs to those with autophagy profiles or those who have an axonal transport problem.”
Antisense oligonucleotide therapy is already impacting the gene therapy landscape for SOD1-associated mutations linked to ALS, the most common of which is C9orf72. SOD1 is in phase 2 human trials and Dr. Harms anticipates C9orf72 to move into clinical trials this year.
“It feels like we’re always on the verge and that something is always just around the corner,” says Dr. Harms. “We are optimistic that genomically characterizing and determining the subtypes of ALS and then pursuing genetically targeted therapies is the most viable idea that we’ve had in a long time.”
ALS Clinical Trials: Bringing Therapeutics Closer to Home
Jinsy A. Andrews, MD, MSc, is Director of Neuromuscular Clinical Trials in the Department of Neurology at Columbia. Prior to joining Columbia, Dr. Andrews was Head of Neuromuscular Therapeutics at Cytokinetics, where she focused on developing novel, small molecule skeletal muscle activators as a potential therapy for neuromuscular diseases, bringing the therapy from phase 1 to phase 3 in clinical trials for ALS, and subsequently, spinal muscular atrophy.
“My experience in industry has enabled me to see beyond the academic development of clinical research,” says Dr. Andrews. “I learned more of the regulatory process and interacted with clinical researchers and experts within the field in the U.S., Canada, and Europe, and also collaborated both nationally and internationally on specific compounds. I characterize my academic development as unconventional and a little bit out of the box, which is how I approach developing clinical trials in ALS and neuromuscular disorders.”
Many of the compounds being tested at Columbia are in phase 2 or phase 3 development and are targeting different mechanisms of motor neuron degeneration, including hyperexcitability in both the peripheral and cortical motor neurons.
Many of the compounds being tested at Columbia are in phase 2 or phase 3 development. The compounds are targeting different mechanisms of motor neuron degeneration, including hyperexcitability in both the peripheral and cortical motor neurons. “These are compounds that are looking at reducing microglial activation or processes involved in its inflammation that might be causing motor neuron degeneration, as well as trying to enhance the activation of the skeletal muscle in the setting of reduced nerve input,” explains Dr. Andrews, who is participating in an international collaboration to gain consensus in updating clinical trial guidelines in ALS.

Dr. Jinsy A. Andrews
According to Dr. Andrews, traditionally, many compounds have targeted different singular mechanisms of motor neuron degeneration. In recent years, however, compounds are being developed to target the neighborhood cells — the astrocytes — as well as the skeletal muscle to enhance the skeletal muscle function, thereby improving physical function in these diseases that are chronic and progressive. Parallel to those efforts, Dr. Andrews is pursuing experimental therapies in clinical trial settings to find a drug that can be effective in mitigating the disease.
“Our group is also involved in epidemiological studies to evaluate environmental risk factors that are associated with the sporadic forms of ALS,” says Dr. Andrews. “For me, it’s about trying to introduce innovation to clinical trials. I am heavily involved in collaborations in developing predictive algorithms or outcomes measures since we don’t have a good way of predicting how the disease progresses in ALS.”
In order to find effective therapies for rare neurological disorders, Dr. Andrews believes the only way is through collaboration. “And not just on a national scale, but an international scale,” she says. “Some of these phase 2 trials may be multicenter national studies, but the phase 3 clinical trials we are conducting are international. There must be a global shift in the way we do clinical trials and engage multiple stakeholders in that development process.”
Related Publications
HIFU: Heralding New Hope for Movement Disorders





