Obesity: Advancing Treatment Through Clinical Trials

Dr. Dympna Gallagher and Dr. F. Xavier Pi-Sunyer
The New York Obesity Nutrition Research Center at Columbia University Medical Center continues to pursue groundbreaking discoveries about the causes, complications, and treatment of obesity that are translating into effective interventions across the lifespan. Established nearly four decades ago, the program is the oldest NIH-funded obesity research center, receiving support from the National Institute of Diabetes and Digestive Kidney Diseases to advance the understanding of obesity.
“Understanding obesity is a challenge because it is multifactorial in nature,” says Dympna Gallagher, EdD, Professor of Nutritional Medicine at Columbia and Associate Director of the New York Obesity Nutrition Research Center. “Our researchers are exploring biological, genetic, epigenetic, behavioral, sociocultural, and environmental factors, as well as potential intrauterine and intergenerational influences. These factors shift and change as a person gains or loses weight and throughout the aging process.”
Distinguished Repertoire of Clinical Research
For more than two decades, Dr. Gallagher and F. Xavier Pi-Sunyer, MD, MPH, Co-Director of the New York Obesity Nutrition Research Center, have been at the forefront of clinical trials to better understand and advance treatment for obesity and its medical consequences.
Diabetes Prevention Program
The co-epidemics of obesity and type 2 diabetes have long been the research focus of Dr. Pi-Sunyer, Professor of Medicine and a faculty member of the Institute of Human Nutrition at Columbia. “Obesity often leads to type 2 diabetes, which has a devastating impact on the individual and the public because it diminishes quality of life and is extremely expensive to manage,” says Dr. Pi-Sunyer. “One of my primary research goals is to find an effective intervention that will prevent the onset of diabetes in overweight or obese individuals.”
Dr. Pi-Sunyer is the site PI of the Diabetes Prevention Program (DPP), an NIH-sponsored clinical trial that has compared intensive lifestyle intervention with dietary changes and increased physical exercise to the use of metformin for preventing type 2 diabetes. “This was the first large-scale study to demonstrate that modest weight loss and increased activity achieved through lifestyle changes could go a long way to prevent type 2 diabetes in high-risk persons,” he explains. “This was such an important research breakthrough that the CDC implemented a lifestyle intervention program that emulated the DPP, which is currently offered at YMCAs across the country and beginning to be offered by other groups around the country and abroad.” Dr. Pi-Sunyer continues to follow study participants through the DPP Outcomes Study to explore the “legacy” effect of intensive lifestyle intervention on the onset of diabetes, microvascular disease, heart disease, and cancer.
Look AHEAD
“We know that type 2 diabetes patients have twice the risk of developing heart disease than non-diabetic persons, so another important research question is whether or not intensive lifestyle intervention can reduce heart events in type 2 diabetes patients,” says Dr. Pi-Sunyer, who also served as the site PI of Action for Health in Diabetes (Look AHEAD), a multisite, intervention trial that compared the effect of intensive lifestyle intervention to diabetes support and education (usual care) in overweight and obese type 2 diabetes patients on the development of cardiovascular disease.
“While the Look AHEAD study was stopped after 10 years because there was no cardiovascular effect, the study illuminated important benefits of intensive lifestyle intervention,” says Dr. Pi-Sunyer. “These included improved biomarkers of glucose and lipid control, less sleep apnea, lower liver fat, less depression, improved insulin sensitivity, less urinary incontinence, less severe kidney disease, reduced need of diabetes medications, maintenance of physical mobility, improved quality of life, and lower costs.” In the Look AHEAD Extension Study, Dr. Pi-Sunyer is assessing the long-term influence of intensive lifestyle intervention on aspects of healthy aging, including cognition and frailty.
As Director of the Human Body Composition Core Laboratory at the New York Obesity Nutrition Research Center, Dr. Gallagher applies her expertise in human phenotyping to investigate the effect of obesity and weight loss on body composition. “I’m interested in what happens when body weight changes respective to adipose tissue and skeletal muscle, which play an important role in metabolic disease and healthy aging,” she says. “In an investigator-initiated study involving a subset of participants in the Look AHEAD study, we found that even the smallest amount of weight loss reduces both visceral and intermuscular adipose tissue deposits, which correlate with improvements in blood pressure, glycemic control, and dyslipidemia.”
In a separate analysis, Dr. Gallagher explored the impact of weight loss on lean muscle mass in elderly participants. “It is important for elderly persons to have sufficient lean muscle in their lower extremities to carry out activities of daily living and avoid fractures,” she says. “We found that after the first year of weight loss, elderly persons lost lean muscle mass, but after the second year, their lean muscle mass was regained in the arms and legs but not in the trunk.”
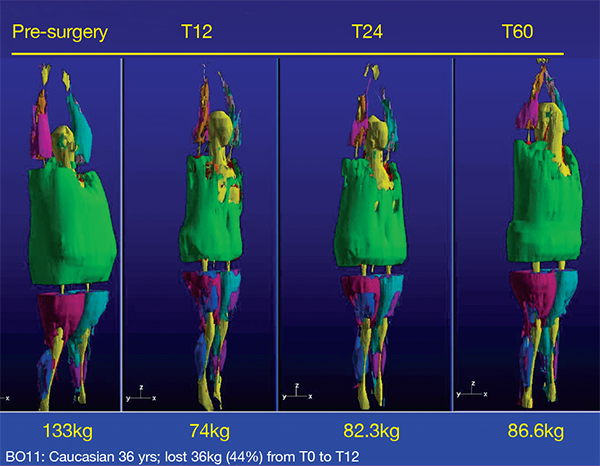
Whole body MRI 3-D volume rendering
(Courtesy of Dr. Dympna Gallagher)
Click here to view larger image
Longitudinal Assessment of Bariatric Surgery
The Longitudinal Assessment of Bariatric Surgery, an NIH-sponsored consortium of six clinical centers, conducted clinical, epidemiological, and behavioral research to assess the effects of bariatric surgery. At Columbia, Dr. Gallagher performed whole-body MRI to measure the impact of bariatric surgery on adipose tissue depots in patients who underwent bariatric surgery at NewYork-Presbyterian. “Our study found a significant reduction in adipose tissue at 12 and 24 months post-surgery, with continued losses in visceral and intermuscular adipose tissue between 12 and 24 months in women, at a time when weight change was not significant. This means that bariatric surgery has a beneficial effect on reducing adipose tissue depots in these women, even after their weight had stabilized,” she explains. “We are now looking at the eight-year data to explore the efficacy of bariatric surgery for long-term weight loss and improvement in obesity-related medical conditions.”
LIFE-Moms
“From a public health standpoint the emphasis on obesity research has to be on prevention, which must start early in life to be effective,” says Dr. Pi-Sunyer, the site co-PI along with Dr. Gallagher of the Lifestyle Interventions for Expectant Moms (LIFE-Moms) Consortium, an NIH-sponsored collaboration of four clinical centers conducting intervention trials on mothers and their neonates. “The aim of LIFE-Moms is to develop methods to prevent women with overweight and obesity from gaining too much weight during pregnancy. These women tend to have children who are prone to overweight and obesity as adults. We are using Lifestyle Intervention for Two [LIFT] and are following the mothers and neonates to determine the impact on gestational weight gain, control of maternal hypoglycemia, return to postpartum weight, and achieving appropriate infant growth.”
“The primary aim of this site-specific study was to investigate the effectiveness of controlling gestational weight gain on neonate body composition, using accurate measures of fat and fat-free mass,” says Dr. Gallagher. “Evidence from epidemiological data suggests that fetal exposure to excessive maternal gestational weight gain may independently influence long-term adiposity-related disease trajectories. Results from our study show that a lifestyle intervention in women with overweight and obesity that targeted the control of gestational weight gain resulted in no differences in fat mass but greater lean mass in the infant at birth. The intervention delivered during the second and third trimesters promoted a healthier pregnancy lifestyle that had an important measurable impact on neonate lean tissue.”
Future Research Goals
“My immediate and future research plans are to further our understanding of the in utero and pre-pregnancy effects on future obesity risk,” says Dr. Gallagher. “Does intervening before a woman gets pregnant have an independent effect on her offspring? Is something being modified in the womb, epigenetic or otherwise, that influences the offspring’s future risk for obesity?”
Another area of interest is that “many elderly people over age 65 are overweight and have risk factors for heart disease, diabetes, and stroke,” says Dr. Pi-Sunyer. “An important controversy is whether it is healthy for elderly people to lose weight, and if so, how can we help them achieve their goals.”
Reference Articles
Gallagher D, Rosenn B, Toro-Ramos T, Paley C, Gidwani S, Horowitz M, Crane J, Lin S, Thornton J, Pi-Sunyer X. Greater neonatal fat-free mass and similar fat mass following a randomized trial to control excess gestational weight gain. Obesity (Silver Spring). [In press]
Gallagher D, Kelley DE, Thornton J, Boxt L, Pi-Sunyer X, et al; MRI Ancillary Study Group of the Look AHEAD Research Group. Changes in skeletal muscle and organ size after a weight-loss intervention in overweight and obese type 2 diabetic patients. The American Journal of Clinical Nutrition. 2017 Jan;105(1):78-84.
Clifton RG, Evans M, Cahill AG, Franks PW, Gallagher D, et al; LIFEMoms Research Group. Design of lifestyle intervention trials to prevent excessive gestational weight gain in women with overweight or obesity. Obesity (Silver Spring). 2016 Feb;24(2):305-13.
Toro-Ramos T, Goodpaster BH, Janumala I, Lin S, Strain GW, Thornton JC, Kang P, Courcoulas AP, Pomp A, Gallagher D. Continued loss in visceral and intermuscular adipose tissue in weight-stable women following bariatric surgery. Obesity (Silver Spring). 2015 Jan;23(1):62-69.
Related Publications





