Download the Full Report View the E-booklet
Read more about our top research and key innovations from 2025:
First-Of-Its-Kind Program Dedicated To Pediatric Robotic Cardiac Surgery
Split-Root Domino Partial Heart Transplant Saves Three Pediatric Patients
Novel Treatment Method Can Address Aggressive Pediatric Brain Tumor
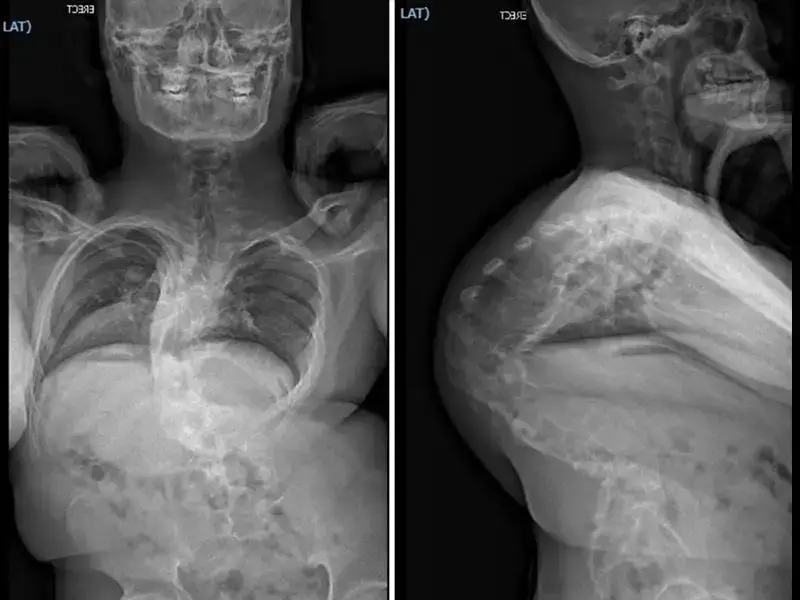
Dual-Specialty Approach Improves Outcomes In Pediatric Spine Cases
Extensive Multistage Spine Surgery Transforms A Severe Case Of Kyphoscoliosis
Research Highlights Critical Gaps In Treating Severe Aplastic Anemia In Children
Addictive Screen Use Linked To Suicidal Behavior In Adolescents
Study Shows Adolescent Depression Rates Spiked During COVID-19
Advancing Pediatric Cornea Care Through A Multidisciplinary Approach
Newborn Gene Sequencing Expands Early Detection Of Treatable Diseases
Landmark Surgery Saves Three Children With One Donor Heart
Gene Therapies Are Revolutionizing Care For Sickle Cell Disease