Download the Full Report View the E-booklet
Read more about our top research and key innovations from 2025:
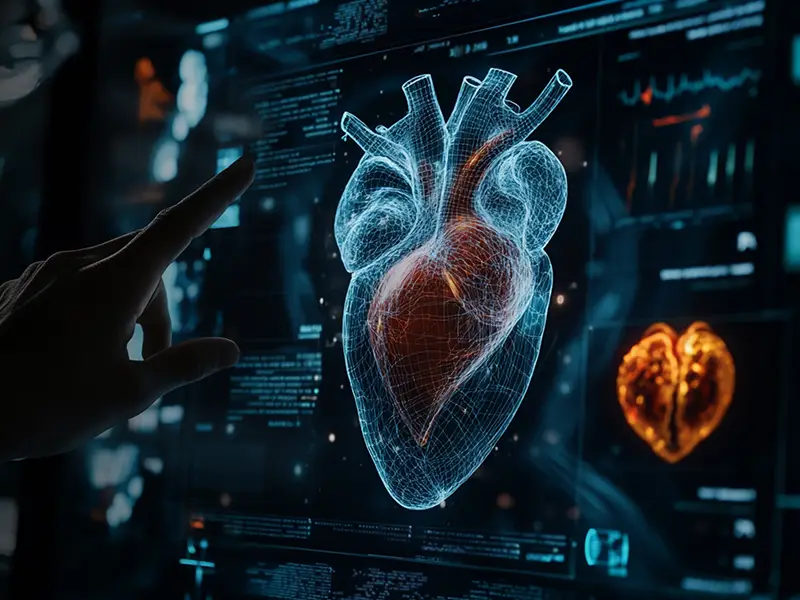
Study Shows Ability Of AI Screening Tool To Detect Structural Heart Disease
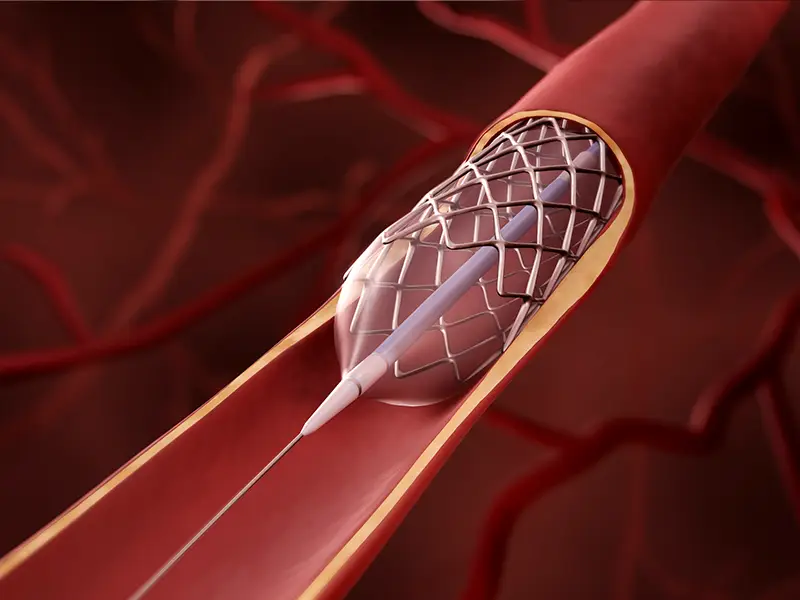
5-Year Outcomes Show PCI Can Be As Effective As Bypass In Treating CAD
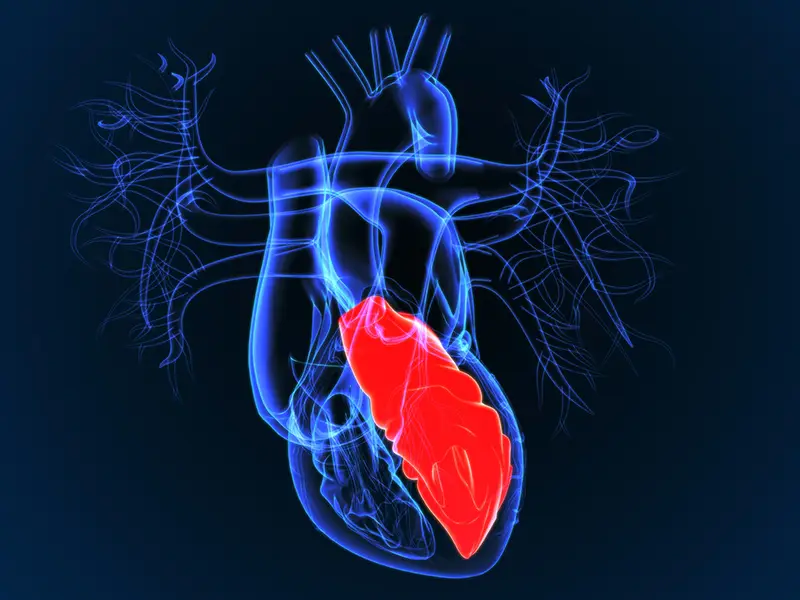
LVAD Therapy Offers Survival Outcomes Similar To Heart Transplant In Younger HF Patients
Integrated Team Performs New York’s First Heart-Lung-Liver Transplant
New Mobile App Makes Heart Failure Education More Accessible
Split-Root Domino Partial Heart Transplant Saves Three Pediatric Patients
Novel Remote Monitoring Device May Detect Heart Failure Events Earlier
GLP-1s Provide New Options To Manage Heart Disease
Advancing Cardiology And Heart Surgery Through Collaboration
Developing Precise Diagnostics For Hypertrophic Cardiomyopathy