For younger patients with heart failure, receiving a left ventricular assist device (LVAD) may be as effective at prolonging life as undergoing a heart transplant or may even increase the net prolongation of life, according to recent research led by Nir Uriel, M.D., MSc, director of heart failure, cardiac transplantation, and mechanical circulatory support at New York-Presbyterian and national co-principal investigator of the MOMENTUM 3 (Multicenter Study of MagLev Technology in Patients Undergoing Mechanical Circulatory Support Therapy with HeartMate 3) study.
The findings were recently published in the Journal of the American College of Cardiology: Heart Failure and first presented in May at Heart Failure 2025, the annual meeting for the European Society of Cardiology’s Heart Failure Association, and they could impact how cardiologists approach treatment strategies for this patient population.
Advancements in mechanical circulatory support and heart transplantation have significantly improved outcomes for patients with advanced heart failure. Yet for patients under 50, who generally have fewer comorbidities and a longer life expectancy, and who tend to be more resilient to the physiologic demands of either therapy, the decision to receive an LVAD or go straight to heart transplantation remains complex.
For many patients, an LVAD-first strategy may be the best of both worlds by offering net prolongation of life.
— Dr. Nir Uriel
“The median survival following heart transplantation in young patients is 14 years,” says Dr. Uriel. “While this represents a significant achievement, it remains relatively short given the patients' young age. To increase the net prolongation of life, we should consider strategies such as introducing LVAD therapy prior to transplantation.”
The findings from Dr. Uriel and his colleagues were based on a comparative analysis of data from the MOMENTUM 3 trial, specifically on trial participants who were younger than 50 at the time of receiving a HeartMate 3 LVAD implant; and from the United Network for Organ Sharing (UNOS) registry on patients who were under 50 at the time of being listed for transplant and who had never had an LVAD.
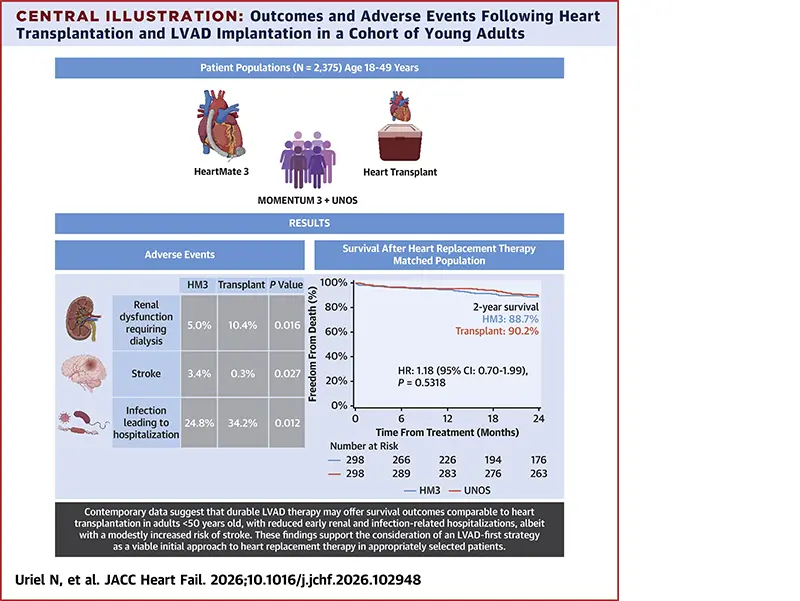
The results of their analysis showed that two-year survival rates between the LVAD and heart transplant groups were 88.8% and 92.2%, respectively, but after propensity score matching, the numbers were essentially the same, at 88.7% and 90.2%. “Our analysis suggests that use of LVAD therapy can offer comparable survival benefits to heart transplantation for this cohort of younger patients,” says Dr. Uriel.
Other Outcomes

Dr. Uriel first presented the findings at Heart Failure 2025 in May.
When compared to patients on the transplant waitlist, LVAD recipients also had significantly better outcomes in most other categories after propensity score matching. At two years, freedom from death or delisting due to worsening clinical status was 90% in the LVAD group, compared to 77% in the waitlisted group. And one-year post-treatment, LVAD recipients experienced fewer infections requiring hospitalization (24.8% vs. 34.2%) and a lower incidence of renal dysfunction requiring dialysis (5% vs. 10.4%). However, the LVAD cohort did experience higher rates of stroke (3.4%) than their transplant counterparts (0.3%).
These findings offer support for a treatment strategy that starts a younger patient on LVAD therapy before bridging to transplant. “For many patients, an LVAD-first strategy may be the best of both worlds by offering net prolongation of life,” says Dr. Uriel. The increased risk of stroke, however, does underscore the need for vigilant neurologic monitoring and optimized anticoagulation management.
Source: Heart Replacement Therapy in Young Patients, JACC: Heart Failure, February 2026
More About MOMENTUM 3
The MOMENTUM 3 trial, launched in 2014, is the largest randomized clinical trial to evaluate LVAD therapy in advanced heart failure, enrolling over 2,200 patients across 69 U.S. sites. NewYork-Presbyterian was one of the first and largest enrollment sites in the trial.
Published in The New England Journal of Medicine in 2018, the two-year findings led to FDA approval of the HeartMate 3 LVAD as a destination therapy, conditional on an extended evaluation to five years of follow-up among those still receiving LVAD support. The five-year results, published in JAMA in 2022, confirmed that LVAD therapy can extend survival to five years or more, well beyond previous benchmarks.
This latest analysis challenges the longstanding preference for heart transplantation in patients under 50 and highlights the need for ongoing real-world data to guide timing and patient selection. Says Dr. Uriel, “These findings continue to support the use of LVADs and reinforce the importance of individualized risk assessment when considering mechanical support in younger patients.”




