Read more about our top research and key innovations from 2024:
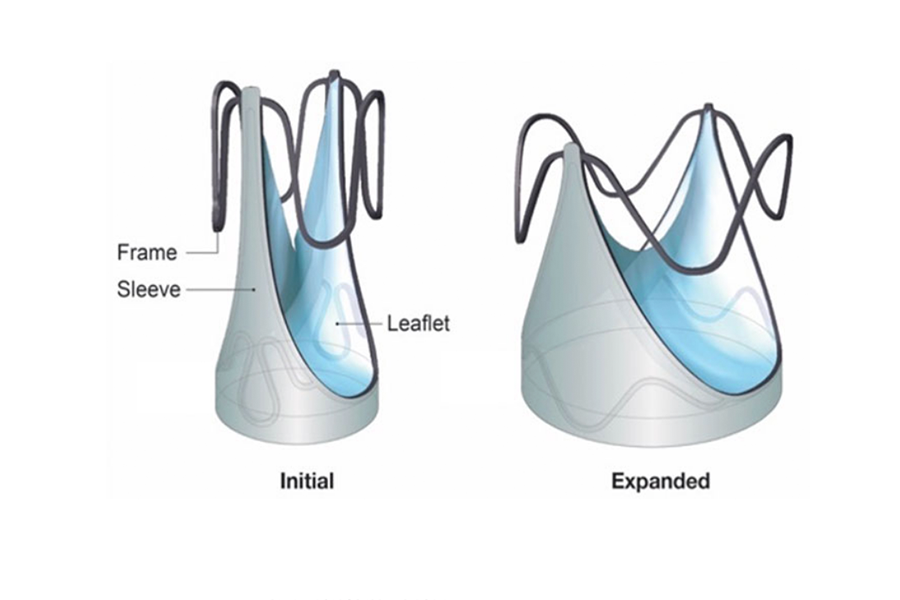
Novel Technology Helps Children with Pulmonary Valve Disease
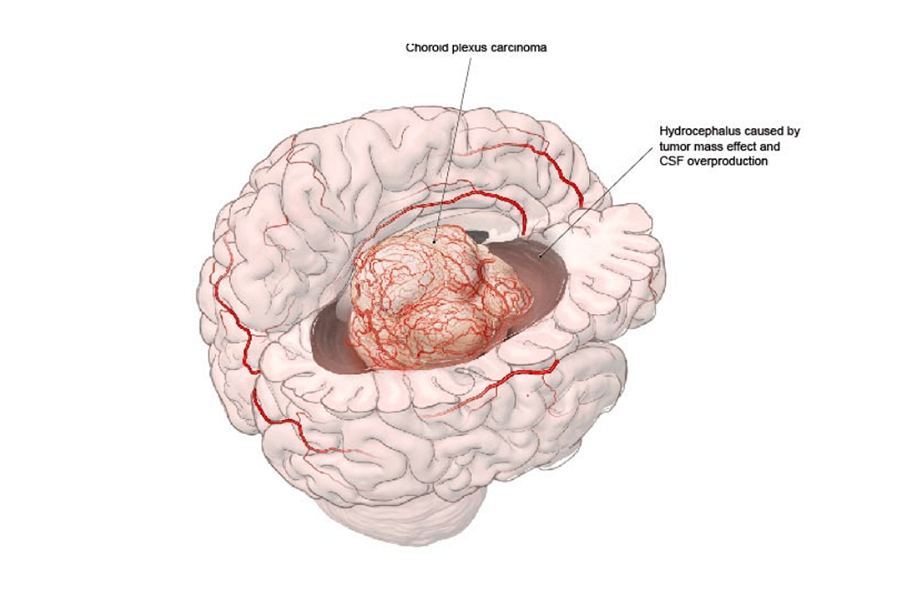
Intra-Arterial Chemo Advances Treatment of Pediatric Tumors
Reducing Waitlist Mortality for Pediatric Liver Transplant
Understanding Co-Occurrence of Celiac Disease & Eosinophilic Esophagitis
The Connection Between Youth Anxiety Disorders & OCS
Against the Odds: Improving Survival for Children with Pulmonary Vein Stenosis
Cracking the Code: Sequencing the Hodgkin Lymphoma Genome to Uncover New Precision Therapies