Read more about our top research and key innovations from 2024:
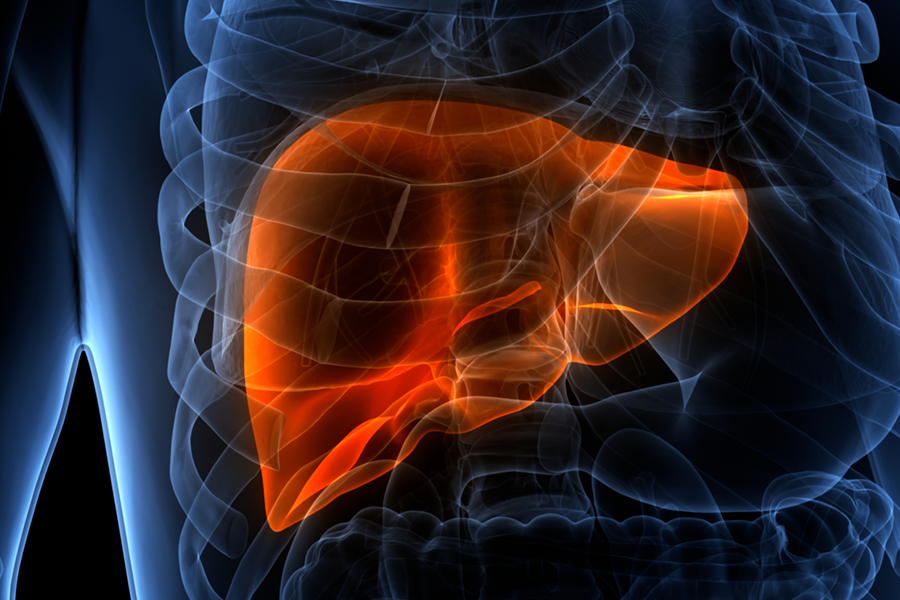
Program Offers Noninvasive Histotripsy for Cancerous Liver Tumors
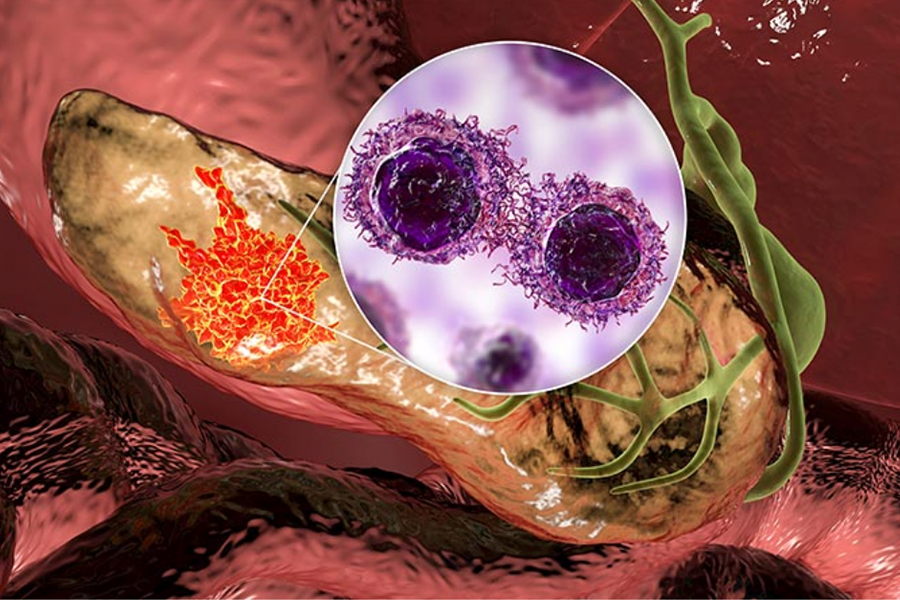
Trial Evaluates Novel Treatment Approach for Pancreatic Cancer
Personalizing Cancer Treatment with Genomics & AI
Multidisciplinary Team Finds Mechanism to Inhibit Metastatic ESCC
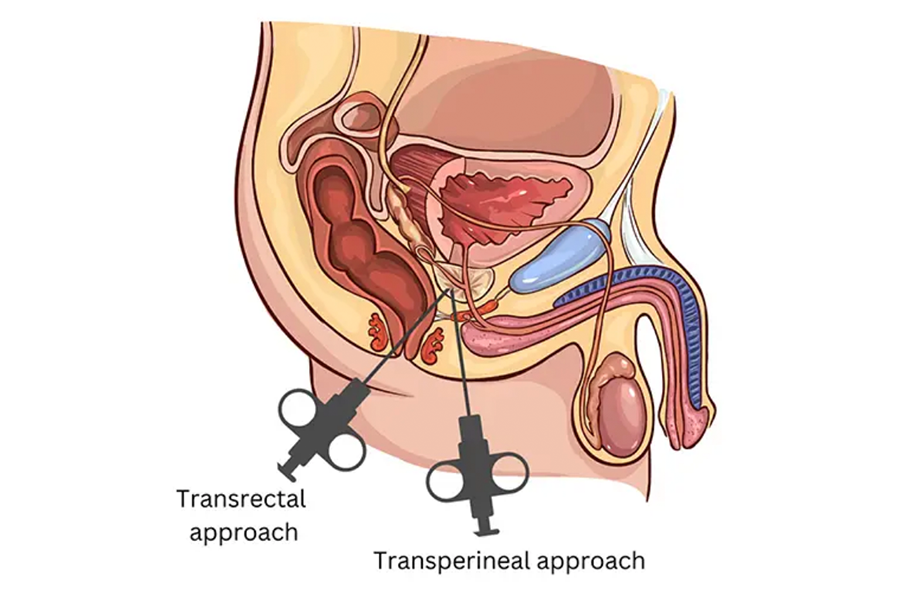
Assessing a New Standard of Care in Prostate Biopsies
Getting Ahead of Cancer: The Life-Saving Power of Cascade Genetic Testing
Connecting Cardio & Cancer: Mitigating Cardiotoxicity with Optimized Treatment Strategies
A Patient-Centered Approach to a Complex Cancer Case