Read more about our top research and key innovations from 2024:
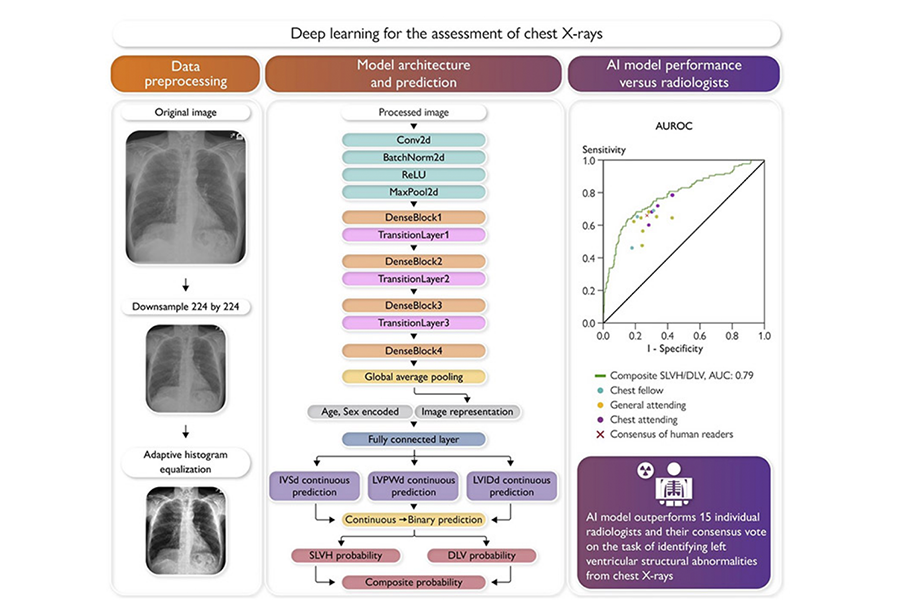
Machine Learning Model Advances Early Heart Failure Diagnosis
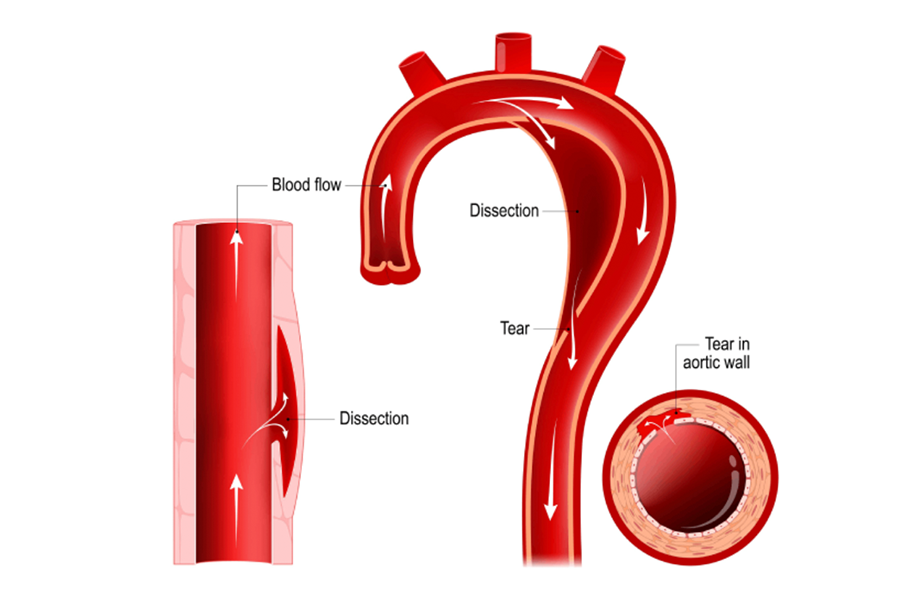
Type B Dissections in Marfan Syndrome Linked to Severe Phenotype
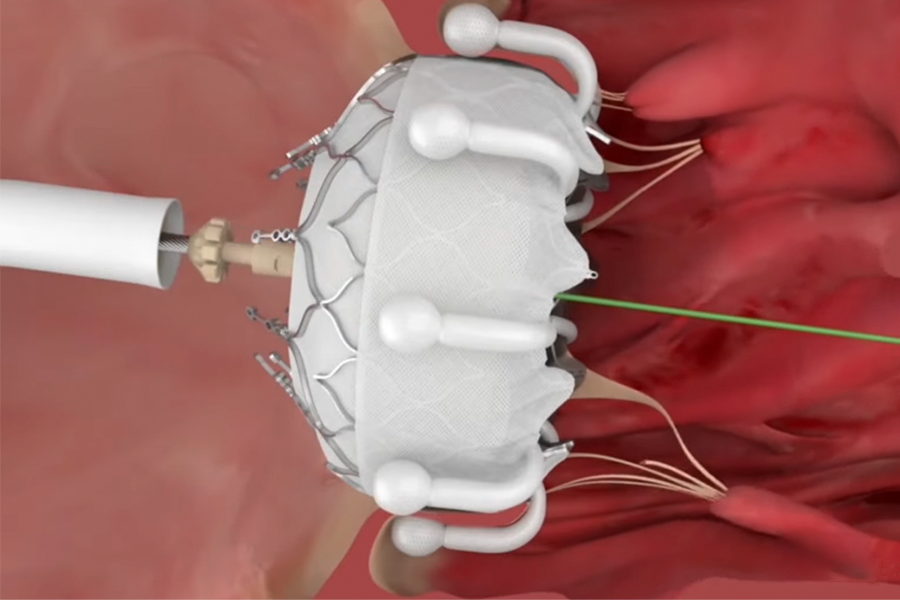
New Center Offers Advanced Care for Valve Diseases
Preop Drug May Reduce Side Effects of Cardiac Surgery
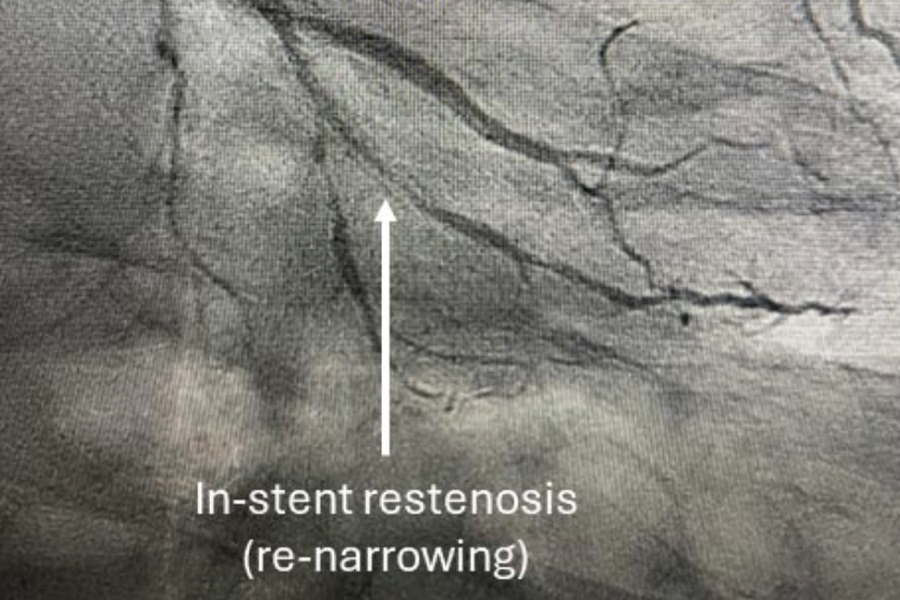
Drug-Coated Balloon Approved for Coronary In‑Stent Restenosis
Reimagining Research: Enhancing Cardiac Care for Underrepresented Populations
The Surgical Robot: Advancing Medicine with Robot-Assisted Technology
Connecting Cardio & Cancer: Mitigating Cardiotoxicity with Optimized Treatment Strategies
Drug-Coated Balloon Approved for Coronary In‑Stent Restenosis