Parallel programs in neurology and neurosurgery at NewYork-Presbyterian/Columbia University Irving Medical Center and NewYork-Presbyterian/Weill Cornell Medical Center strengthen and extend our ability to offer the most advanced technologies, newest therapies, and interdisciplinary approaches for the most challenging brain, neurological, and spinal disorders. The Neurology and Neurosurgery faculty of Columbia University Vagelos College of Physicians and Surgeons and Weill Cornell Medicine continue to explore and develop diagnostic, interventional, and surgical approaches to optimize outcomes.
NewYork-Presbyterian Hospital’s neurology and neurosurgery programs – ranked #3 in the country by U.S.News & World Report – make it a destination for patients from around the world.
MMA Embolization: Advancing Treatment for Subdural Hematoma
New Gene May Drive Earliest Brain Changes in Alzheimer’s Disease
Focused Ultrasound Targets Refractory Epilepsy
New Approaches for Treating Aneurysms
Uncovering Mechanisms of Vascular Disease in Obstructive Sleep Apnea
MMA Embolization: Advancing Treatment for Subdural Hematoma
A Weill Cornell neurosurgeon and interventional neuroradiologist who pioneered the middle meningeal arterial (MMA) embolization technique for chronic subdural hematoma as a first-line alternative to craniotomy has now performed over 300 of these procedures with a complication rate of less than one third of 1 percent. Recruitment is now underway for a clinical trial led by Weill Cornell that incorporates 40 centers in the United States and is expected to be a sentinel trial solidifying MMA embolization as the standard of care to address the most common yet complex type of intracranial hemorrhage.
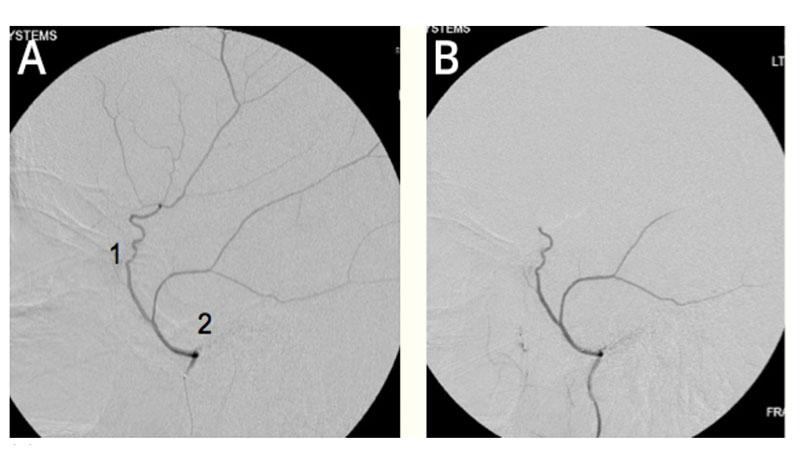
(A) Common configuration of the middle meningeal artery with a common trunk that divides into frontoparietal (1) and squamosal/temporal (2) branches. (B) With this configuration, embolization can be performed with the microcatheter tip proximal to the bifurcation of these branches to achieve safe embolization of the maximal amount of dura.
New Gene May Drive Earliest Brain Changes in Alzheimer’s Disease
Columbia researchers have identified an Alzheimer’s gene that may drive the first appearance of amyloid plaques in the brain. Some variants of the gene, RBFOX1, appear to increase the concentration of protein fragments that make up these plaques and may contribute to the breakdown of critical connections between neurons. The investigators examined the genomes of nearly 4,300 people whose PET images revealed amyloid deposits but who had not yet developed Alzheimer’s symptoms. The finding could lead to new therapies that prevent Alzheimer’s and better ways of identifying people with the greatest risk of developing the disease.
Illustration of the processes leading to the formation of amyloid plaques characteristic of Alzheimer's disease
Focused Ultrasound Targets Refractory Epilepsy
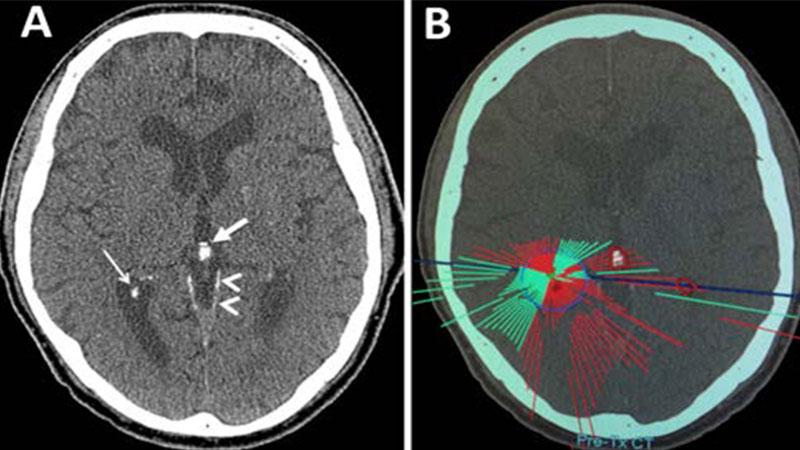
Weill Cornell neurosurgeons, innovators in the application of high-intensity focused ultrasound (HIFU) for the treatment of essential tremor, are now using this therapy for patients with refractory epilepsy. HIFU is transforming treatment by gaining access deep within the brain without harming healthy tissue, enabling surgeons to ablate targeted tissue without exposing the brain to the effects of ionizing radiation. Patients often require two or three craniotomies to target these small, white matter tracts. This noninvasive method to achieve the therapeutic goal presents a lower risk to patients.
MRgFUS treatment plan of a study patient accounting for intracranial calcifications. A: Axial noncontrast image showing dural (arrowheads), choroid plexus (narrow arrow), and pineal (wide arrow) calcifications in the region of the treatment target. B: Pretreatment plan demonstrating ultrasound elements reaching target (green) and being blocked (red) due to intracranial calcifications. Patient had inadequate element availability secondary to intracranial calcifications.
New Approaches for Treating Aneurysms
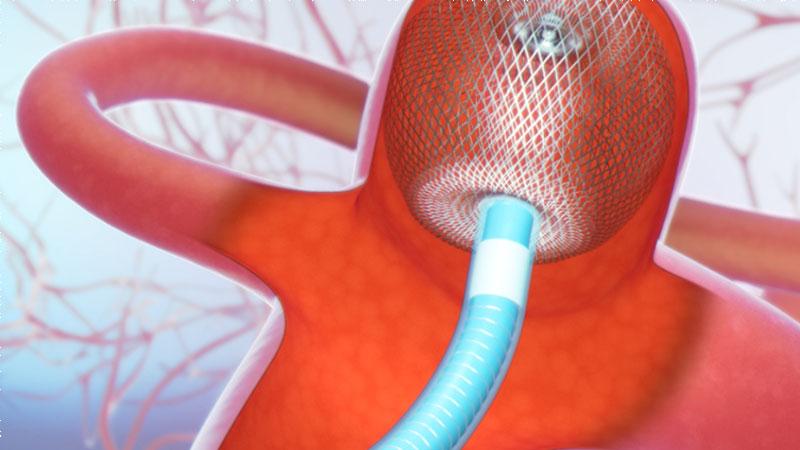
Columbia and Weill Cornell neuroendovascular surgeons continue to explore and refine techniques to treat brain aneurysms, including flow diverter systems. They were among the first in the nation to use the Woven EndoBridge (WEB®) Aneurysm Embolization System, a permanent nitinol self-expanding mesh ball implant for the treatment of wide-neck intracranial aneurysms located at or near branching areas of arteries in the brain. A completely new approach to the treatment, the WEB device fills up the aneurysm and diverts blood flow from the aneurysm. What may otherwise have required a craniotomy to surgically clip the aneurysm can now be performed quickly with minimal recovery time. Results are preliminary but very promising, according to the researchers.
Woven EndoBridge (WEB) Aneurysm Embolization System

Uncovering Mechanisms of Vascular Disease in Obstructive Sleep Apnea
Weill Cornell neurologists led a multicenter study in collaboration with the National Institutes of Health to investigate mechanisms of vascular disease in obstructive sleep apnea to determine potential interventions. Their objective was to establish whether increased platelet activity is altered in patients with obstructive sleep apnea with intermittent nocturnal hypoxemia. Characterizing these mechanisms will lead to a better understanding of the pathways involved in the development of cardiovascular disease and help identify potential therapeutic strategies targeting the reduction or avoidance of endothelial injury in order to reduce the morbidity and mortality associated with sleep apnea.
Scanning electron micrograph of an activated platelet

Overactive Brain Waves Trigger Essential Tremor
A new study by Columbia investigators suggests that essential tremor is caused by an abnormally high number of synapses between two types of nerve cells in the brain’s cerebellum – climbing fibers and Purkinje cells. The formation of these synapses appears to be influenced by glutamate receptor delta 2 (GluRẟ2). When this protein is under-expressed, excess synapses that form are not eliminated, resulting in too many neuronal connections. The researchers’ findings raise the possibility of treating the disorder with neuromodulation techniques, such as transcranial direct-current stimulation or transcranial magnetic stimulation to calm the oscillations.
Patients with essential tremor develop excessive cerebellar oscillations; (left) a cerebellar EEG in a control subject and (right) shows additional brain waves in a patient - highest intensity is colored in red, lowest intensity in blue.



