Accelerating Progress in Aortic Disease Management
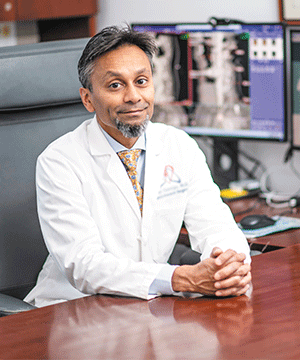
Dr. Virendra I. Patel
Virendra I. Patel, MD, MPH, Chief of Vascular Surgery and Co-Director of the Aortic Center at NewYork-Presbyterian/ Columbia University Irving Medical Center, and his colleagues are advancing the endovascular management of acute aortic dissection. “With recent FDA approval for the use of a new endovascular stent, we now are able to manage acute type B dissections of the descending thoracic aorta in a novel, less invasive way that will greatly impact a patient’s quality of life and longevity,” says Dr. Patel. “The stent graft is delivered through an incision in the groin to reach the entry tear, where it expands to prevent the aorta from rupturing and make a new path for the blood to flow.”
“We have published extensively on the benefits of early intervention in the acute and subacute phase of acute type B aortic dissection,” continues Dr. Patel. “Even in uncomplicated type B dissections, there are clear benefits of aortic remodeling and reduction of late aortic events, specifically ruptures and thoracoabdominal aneurysms. Five-year aneurysm-related mortality is lower in patients who have early interventions for these dissections.”
In collaboration with cardiothoracic surgeon Hiroo Takayama, MD, PhD, Co-Director of the Aortic Center, Dr. Patel performs hybrid aortic arch reconstructions with the frozen elephant trunk technique. “The first device for a complete aortic arch endovascular replacement is now available in the United States, going into its second stage feasibility study,” says Dr. Patel. “Because of our collaborations and high volume, we will be the only center participating in this trial in New York City and one of only three centers on the East Coast. This is a completely minimally invasive replacement of the arch in patients with the appropriate anatomy.”
“Current devices used in treating the aortic arch when the ascending aorta is diseased can be a source of a new dissection or injury due to the large size of the stent,” explains Dr. Patel. “Generally, in these patients, we replace the ascending aorta and create the anatomy for the appropriate landing zone for the arch device so that it lands safely in the prior graft. What is interesting in terms of the hybrid perspective related to the new device is that it allows us to fully replace the aortic arch while limiting the risks associated with the subtotal or total arch replacements in patients with acute dissections and large ascending or aortic arch aneurysms. So, this new trial is going to be very exciting.”
Enrollment criteria include patients with an ascending or aortic arch aneurysm deemed too high risk for open surgery; patients with a previous median sternotomy, which would make the re-entry into the chest a bit more treacherous; and those who have an inadequate landing zone or prior graft replacement of the ascending aorta.
A Hand-Drawn Surgical Blueprint
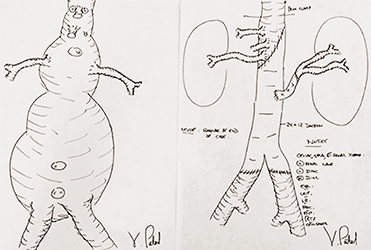
Dr. Virendra Patel Hand-Drawn Surgical Blueprint
In planning for a complex aortic surgery, Dr. Virendra Patel will draw detailed before and after sketches of the aorta to prepare him for where he may encounter problems. “Looking at the scans, I’ll plan where I think the safe sites are to clamp the aorta without showering debris, where I think the anatomy is going to be tricky, and what arteries I’m going to reattach versus keep together,” says Dr. Patel. “I do this for all complex aneurysms. I absolutely think it helps impact recovery. The faster you do the operation, the better you do your organ protection, and the better and quicker the recovery.”



