Shoulder, Elbow, & Sports Medicine
Underscoring Concerns in Shoulder Surgery
Periprosthetic Shoulder Infection
Although uncommon, periprosthetic shoulder infection is a devastating complication often requiring revision surgery and antibiotic treatment. Its diagnosis can be difficult due to the indolent slow growing P. acnes infections that are common to the shoulder. The suspicion of infection is derived from clinical symptoms of pain and stiffness, laboratory exam of inflammatory markers, radiological studies, and microbiological cultures and detection methods.

Dr. William N. Levine
To analyze periprosthetic shoulder infection rates, our orthopedic faculty undertook a retrospective chart review of primary shoulder arthroplasty in patients over a four-year period at NewYork-Presbyterian/Columbia. A total of 695 patients were included in the study; periprosthetic infections occurred in six patients. The overall periprosthetic infection rate for patients undergoing primary shoulder arthroplasty was 0.9 percent. “Both anatomic and reverse shoulder replacement are at risk for infection,” says William N. Levine, MD, Chairman of the Department of Orthopedic Surgery. “Understanding the rates and causes of periprosthetic shoulder infection as well as the treatment costs will help identify areas for system improvement and prevention.”
Assessing Glenoid Components
One of the most common reasons for total shoulder arthroplasty failure is glenoid loosening, which may occur if retroversion is not corrected to <10°. However, accurately measuring postoperative glenoid component version has been difficult without postoperative CT, which adds cost and radiation exposure outside of the standard radiographic follow-up. Dr. William Levine, Dr. Charles M. Jobin, and their colleagues proposed a new method for assessing glenoid components using only routine preoperative CT and postoperative X-rays. The researchers measured preoperative glenoid version using established methods with an axillary X-ray, 2-dimensional CT, and Glenosys software. Postoperative glenoid component version and inclination were measured using Mimics software with preoperative CT and postoperative X-rays.
“This method allows for preoperative planning based on 3D CT models as well as determination of postoperative glenoid version without imaging outside the current standard of care,” notes Dr. Levine. “To our knowledge, this is the first study of this software application in total shoulder postoperative implant positioning.
We hypothesize that coupling routine imaging with Mimics software is as accurate as a postoperative CT scan in determining glenoid component retroversion. Measuring postoperative glenoid component retroversion, and therefore determining how successful surgeons are in correcting excessive retroversion, has the potential to be an important step in understanding the factors that affect glenoid component longevity and loosening.”
As reported in the September 2018 issue of the Journal of Shoulder and Elbow Surgery, the researchers concluded that glenoid component retroversion can be accurately measured with this method, validated to within 1.9° of the gold standard postoperative CT measurement. Future studies using this method may correlate glenoid retroversion correction with glenoid component longevity to help optimize shoulder arthroplasty outcomes.
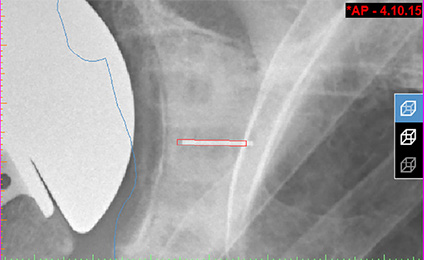
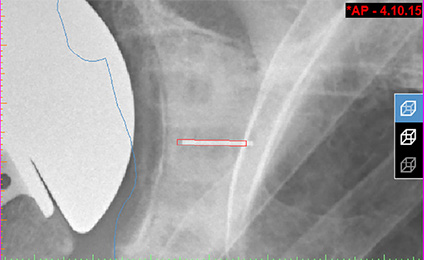
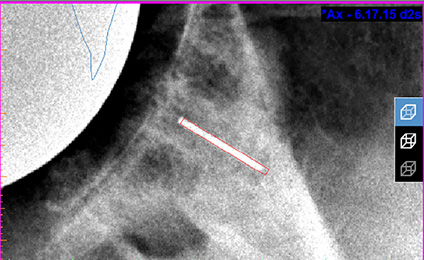
(Left) By aligning the postoperative anteroposterior and axillary X-rays with the projected silhouette of the preoperative 3D scapula model (center and right), the position of the glenoid component metal marker can be determined with respect to the preoperative 3D scapula model. Once this position has been determined, glenoid component version can be measured.
Outcomes and Quality Metrics
Clinical Quality: Shoulder Procedures 2017
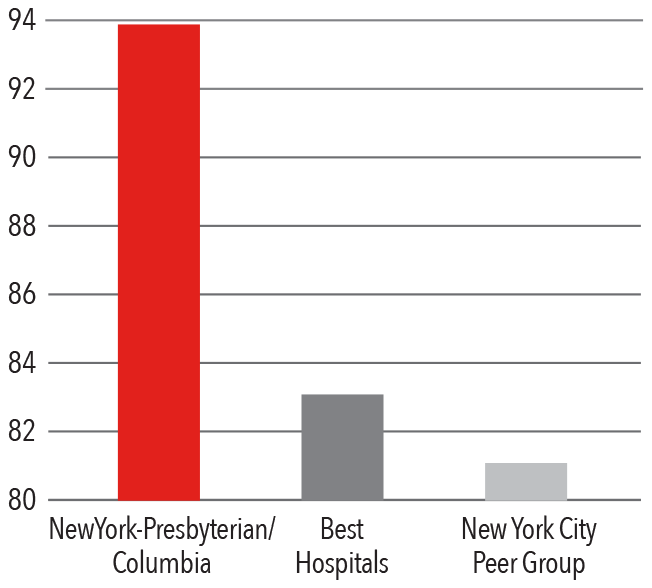
Periprosthetic Shoulder Infection 2012 - 2016
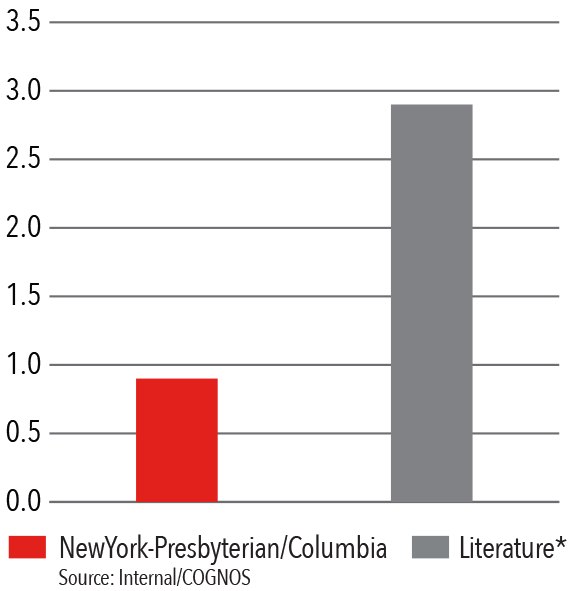
*Literature Source: Franceschini, V et al.
Periprosthetic shoulder infection.
The Open Orthopaedics Journal. 2013 June; 7: 243-49
Columbia Orthopedics has lower infection rates for primary shoulder arthroplasty than rates cited in national peer-reviewed articles.
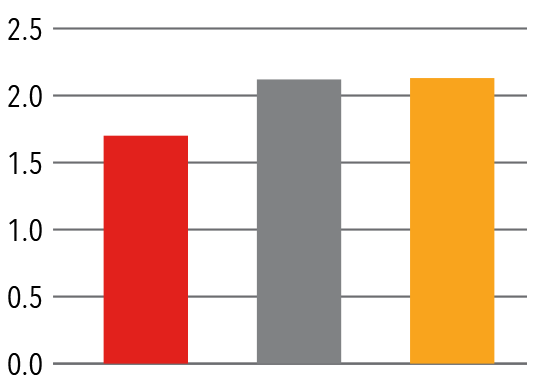
Case Mix Index Medicare
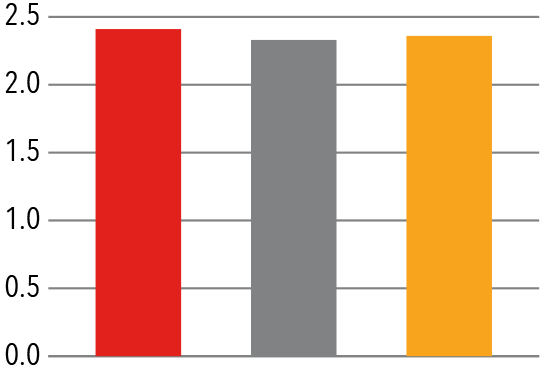
Case Mix Index Non-Medicare
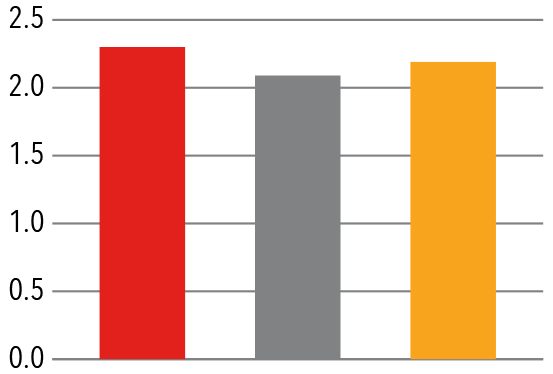
Mortality Index

Length of Stay (In Days)
Addressing Athletic Injuries
Tommy John Surgery: A Rite of Passage?
According to Christopher S. Ahmad, MD, Chief of Sports Medicine and head team physician of the New York Yankees for the past decade, Tommy John surgeries are becoming so widespread, if not routine, in the major leagues that players think it is a rite of passage. “Velocity is the most direct link to the force on the ulnar collateral ligament, and every year the average fast ball velocity is increasing in major league baseball leading to more UCL injuries and Tommy John surgeries,” says Dr. Ahmad, who has researched this topic extensively. “In one study, we looked at pitchers who had thrown complete games and compared them to a control group — pitchers on a major league level who did not throw a complete game — and we found something astonishing. If a pitcher throws a complete game, the chances of going on the disabled list is 74 percent. A control group of players never having thrown a complete game go on the disabled list at a rate of 20 percent.”

Dr. Christopher S. Ahmad
Dr. Ahmad has also raised concerns over the prevalence of UCL surgery among youth athletes, who are also throwing with more velocity and more volume. “It is now obvious that youth athletes are at disturbing risk for throwing-related injuries,” says Dr. Ahmad, who notes that the 17- to 18-year-olds are needing UCL surgery the most. “In fact, major league baseball clubs are consistently drafting young players who have already had ulnar collateral ligament reconstruction, and the number continues to rise.”
The Pitch Registry
Supported by Major League Baseball, Dr. Ahmad has established The Pitch Registry to better understand pitching injuries and how they can be prevented and to serve as a platform for research and education. “This will be a powerful research tool where any athlete who gets injured at any level — major league, college, high school, or even younger — will be enrolled in this registry,” notes Dr. Ahmad. “The registry will provide amazing amounts of data that will give us answers that we can then use to educate parents, coaches, and players.”
Measuring postoperative glenoid component retroversion has the potential to be an important step in understanding the factors that affect glenoid component longevity and loosening.
UCL Tears and Athletic Hip Injuries
A study by Dr. Ahmad and his sports medicine colleagues sought to determine whether professional baseball pitchers who underwent UCL reconstruction had an increased incidence of hip or groin injuries four years before or after surgery. The researchers hypothesized that MLB pitchers who sustain hip or groin injuries may be more likely to develop UCL tears because of alterations and overcompensation in the kinetic chain during overhand throwing. In a study sample of 145 MLB athletes who underwent UCL reconstruction between 2005 and 2017, 40 (27.6 percent) endured a proximal lower extremity injury within four years of their surgery; 16 pitchers sustained hip injuries; 13 suffered hamstring injuries; and 14 experienced groin injuries.
The results of the study, published in the October 2018 online issue of the Orthopaedic Journal of Sports Medicine, demonstrate that MLB pitchers who required UCL reconstruction sustained a higher frequency of proximal lower extremity injuries both before and after surgery compared with matched controls. This finding is significant as the treatment of antecedent hip lesions, as well as an emphasis on hip and core muscle mobility and strengthening, may help reduce injuries to the UCL.
Improving Safety and Quality in Surgical Procedures
Preventing Venous Thromboembolism
Faculty in the Department of Orthopedic Surgery undertook a retrospective analysis of 110 consecutive patients undergoing shoulder, elbow, or sports surgery at NewYork-Presbyterian/Columbia in September 2017 to examine adherence to prophylaxis for venous thromboembolism (VTE). Patients were prescribed VTE prophylaxis based on surgeon preference. Medical records were reviewed to determine the patients’ VTE risk severity score using an adaptation of guidelines from the American College of Chest Physicians. Patients were stratified into three groups — low, moderate, or high risk — based on medical history, injury, and surgery performed. Records were then reviewed to determine if the appropriate postoperative VTE prophylaxis was prescribed based on risk severity score. For each patient who did not receive the appropriate VTE prophylaxis, the treating surgeon was asked if they would have prescribed the recommended VTE prophylaxis if they had known the patient’s risk score.
Of the 110 patients, 101 (92 percent) received the recommended postoperative VTE prophylaxis. Nine patients (8 percent) received less VTE prophylaxis than was recommended. If provided a VTE risk severity score before surgery, surgeons would have administered more aggressive DVT prophylaxis for all nine of these patients. There were no cases of documented or suspected VTE in any of the 110 patients in this study. The researchers concluded that individual surgeon prescribing patterns of postoperative VTE prophylaxis after sports-related orthopedic surgery does not follow standard guidelines nor adequately account for known VTE risk factors. Universal adoption by sports surgeons of a VTE risk severity score to guide VTE prophylaxis could minimize variation, improve recognition of VTE risk factors, and likely improve patient care.
Reoperation Rates for Shoulder Arthroplasty
Reoperation rates are an important measure of quality of care, cost-effectiveness, and key metrics for hospital performance. Healthcare payers increasingly determine reimbursement based on quality and may consider reoperation rates after joint arthroplasty an indicator of quality. With limited data available on 30-day reoperation rates after primary shoulder arthroplasty, our orthopedic surgeons undertook a study to evaluate the 30-day reoperation rates performed at NewYork-Presbyterian/Columbia. Culling data from Columbia’s shoulder arthroplasty registry to identify primary shoulder arthroplasties performed from January 2016 through December 2016, the researchers reviewed patient characteristics, primary diagnosis, and procedure performed, excluding revision arthroplasty cases.
Of the 209 primary shoulder arthroplasties performed during that year, one (0.4 percent) patient was identified as undergoing a reoperation — an evacuation of a hematoma — within 30 days of the primary arthroplasty. Healing following the patient’s reoperation was uneventful with no detectable reduction in outcome compared to patients without a reoperation.
The study suggests that reoperating in the short-term after shoulder arthroplasty appears to be very rare and limited to either traumatic events or hematomas in the setting of anticoagulation use in patients with thromboembolic disease. However, as healthcare expenditures continue to be optimized and reimbursements linked to value and quality of care, both payers and providers need to develop systems to minimize the risk of reoperation. This study serves as an initial benchmark for performance and quality improvement in primary shoulder arthroplasty.
Patient Satisfaction 2017
HCAHPS Communication with Doctors
Retirement After Concussion: Standardizing Decision-Making
Orthopedic and neurology faculty at Columbia collaborated on research related to medical retirement from sports after concussion published in the February 2018 issue of Neurology Clinical Practice. The authors detail a potentially game-changing algorithm based on real patient cases that could standardize medical retirement decisions for athletes suffering from sports-related concussion.
“I think this proposed algorithm is the start of an important conversation that should be had in the sports medicine community,” says Natasha N. Desai, MD, a nonoperative sports medicine specialist at Columbia. “There are many studies and guidelines about the diagnosis of concussion, but there is relatively little out there to guide us in our decision-making in how to approach medical retirement from their sport with our patients. So many factors should be taken into consideration, and it is not a one size fits all. I foresee this algorithm continuing to evolve and improve but it is a great start and has already aided me in my approach to this very difficult conversation.”
Return to Sport Contraindications
| Absolute Contraindications | Relative Contraindications |
| Diffuse axonal injury | Symptoms or signs (including focal neurologic deficit) >90 days without alternate diagnosis |
| Other stuctural abnormality conferring signicant risk of bleed or concerning for prior traumatic brain injury | Diminished academic performance or engagement |
| Decresased threshold/decreased interval |
Elevating Sports Medicine Care at NewYork-Presbyterian Lawrence Hospital
In 2018, Columbia’s Department of Orthopedic Surgery established a world-class Sports Medicine program at NewYork-Presbyterian Lawrence Hospital, under the direction of David Kovacevic, MD. The new program offers comprehensive, interdisciplinary care for both operative and conservative approaches to help restore function and mobility to patients of all ages and athletic ability.

Dr. Jeffrey A. Geller, Chief of the Division of Hip and Knee Reconstruction at NewYork-Presbyterian/Columbia and Chief of Orthopedic Surgery at NewYork-Presbyterian Lawrence Hospital, and Dr. George J. Zambetti discuss a case in a new state-of-the-art operating room at NewYork-Presbyterian Lawrence.
Dr. David Kovacevic specializes in advanced shoulder and elbow repair, complex reconstruction, and joint replacement. Dr. Kovacevic, who cared for the New York Yankees during his fellowship at NewYork-Presbyterian/Columbia, also draws on his experience as head team physician for Yale Men’s and Women’s Rugby in caring for elite athletes.
Elan L. Goldwaser, DO, is an interventional sports medicine specialist and primary care orthopedist who emphasizes noninvasive treatment modalities, including injection-based therapies, medications, and orthobiologics, such as platelet-rich plasma and stem cell injections. Dr. Goldwaser serves as team physician for the US Ski and Snowboard Association, ringside physician for the New York State Athletic Commission, and concussion consultant for The Hackley School.

Dr. Charles M. Jobin
Charles M. Jobin, MD, specializes in treating shoulder and elbow disorders in adults, with expertise in performing total joint replacements, as well as minimally invasive, arthroscopic procedures. Dr. Jobin is the team physician for Riverdale Country School and tends to the orthopedic needs of rugby, lacrosse, and club sports players at Columbia University.
Charles A. Popkin, MD, focuses his practice on sports-related musculoskeletal injuries and conditions affecting the pediatric, adolescent, and collegiate athlete, and in particular, overuse injuries in children resulting from early sports specialization. Dr. Popkin serves as team physician for a number of varsity teams of the City College of New York and as an orthopedic consultant to Mercy College and Sarah Lawrence College.
Dr. Elan L. Goldwaser, Dr. David Kovacevic, and Dr. Charles A. Popkin
George J. Zambetti Jr., MD, is a leader in the field of sports medicine and a seasoned orthopedic surgeon with 37 years of experience treating adult and adolescent patients. Dr. Zambetti specializes in sports-related injuries, arthroscopic surgery, arthritis, and trauma/fractures and has served for decades as team physician for Fordham University Athletics and other institutions.



