Hip & Knee Reconstruction
NewYork-Presbyterian/Columbia is a premier destination for comprehensive care of conditions affecting the hip and knee and serves as a major referral center for patients from this country and abroad. On average, the highly specialized hip and knee surgeons of the Division of Hip and Knee Reconstruction perform more than 1,200 total, partial, and revision hip and knee replacements each year — a high volume that correlates to lower rates of complications and improved outcomes.

Dr. Jeffrey A. Geller, Chief of Hip and Knee Reconstruction at NewYork-Presbyterian/ Columbia University Irving Medical Center, also leads the new Orthopedics and Sports Medicine program at NewYork-Presbyterian Lawrence Hospital.
Division faculty have furthered fellowship training in lower extremity arthroplasty, providing a highly specialized knowledge and skill set focused on the treatment of osteoarthritis, lower extremity deformity, and fragility fractures. Our team of joint specialists is internationally known for applying advanced minimally invasive and traditional surgical techniques and nonsurgical treatment methods to correct hip and knee disorders. In addition to incorporating the most advanced technology and innovative techniques to restore mobility and function, the Division's physician-scientists remain on the cutting-edge of translational and clinical research.
Applying Advanced Technologies and Techniques
The Division’s treatment facilities are equipped with state-of-the-art MRI, CT, and low-radiation EOS imaging. Patients undergoing joint replacement surgery benefit from preoperative measurements for implant design, size, and positioning, individualizing each procedure. Our surgeons often perform robotically assisted procedures to increase accuracy of implant positioning, minimize incision size, and facilitate greater functional outcomes. They are particularly skilled in tissue sparing techniques that optimize instrumentation and leg positioning to accomplish true minimally invasive surgical (MIS) reconstructions.
Our surgeons have expertise and experience in open and minimally invasive surgery using approaches that include direct anterior, Watson-Jones MIS anterolateral, and rarely, the older posterior hip replacements and resurfacings. Using the most advanced image-guided approaches for minimally invasive surgery have resulted in lower rates of infection and faster recoveries. Our surgeons have particular expertise in anterior-based approaches , which they perform for nearly all hip replacement surgery. This minimally invasive method is significantly less disruptive to the surrounding muscles and soft tissues, results in less postoperative pain and decreased risk of hip dislocation, and expedites recovery. Our surgeons are now able to send many patients home the same day, without an overnight hospital stay, using this approach.
Revision Hip and Knee Surgery
About 10 percent of all hip and knee procedures performed by Columbia's orthopedic surgeons are revision surgeries, with the majority of the initial surgeries performed at other institutions. Complications that are commonly addressed include periprosthetic joint infection, instability, adverse local tissue reaction in the setting of metallosis or trunnionosis, mechanical malalignment, incorrect sizing, leg length discrepancy, implant loosening, bearing surface wear, corrosion, and deformity. Our surgeons perform both one-stage and two-stage hip and knee revisions to reduce the possibility of reinjury or reinfection of the joint.
Outcomes and Quality Metrics
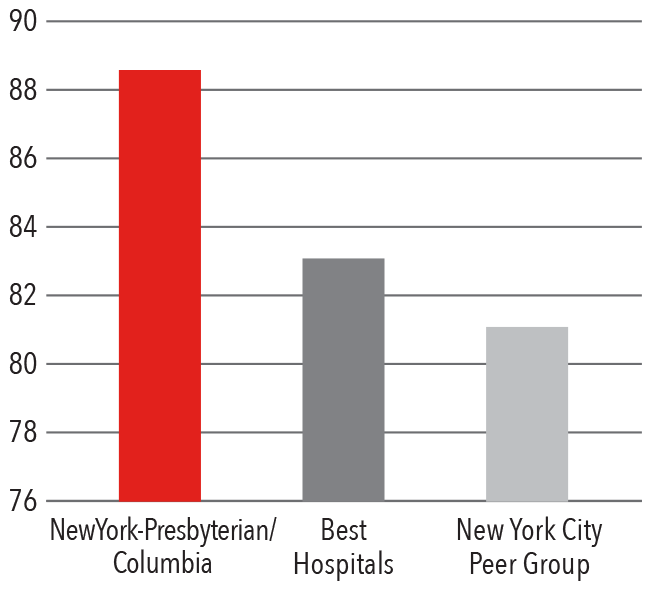
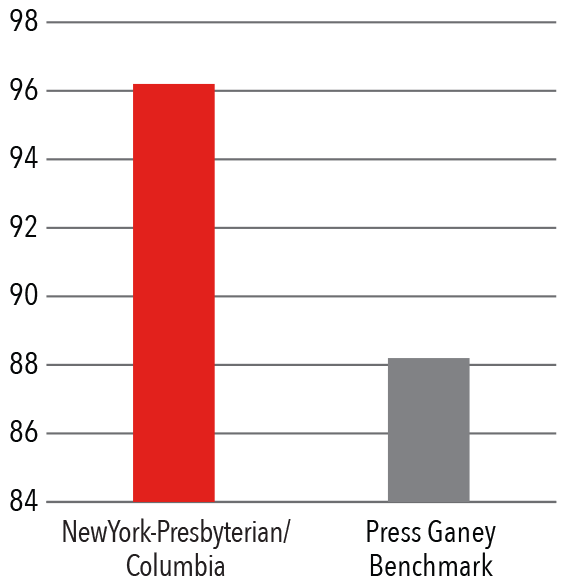
Patient Satisfaction 2016 - 2017
HCAHPS Communication with Doctors
Press Ganey Physician Score
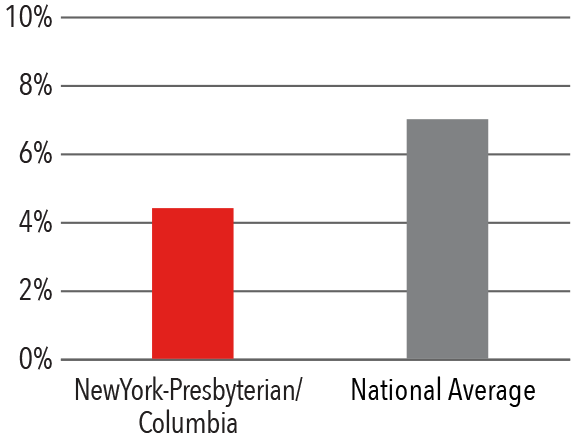
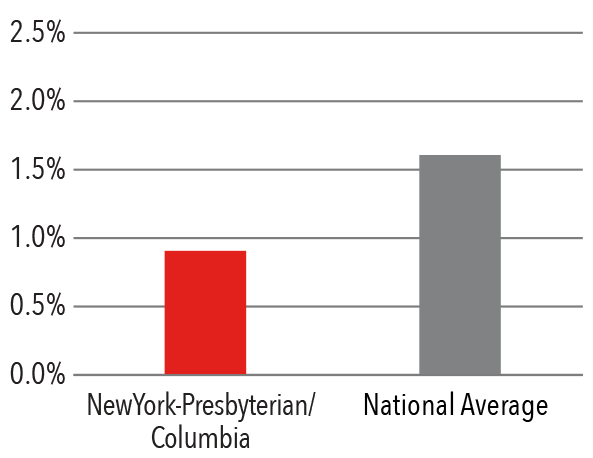
Clinical Quality 2017
90 Day Readmission Rate
90 Day Complication Rate
Hip Prosthesis Surgical Site Infection Rate
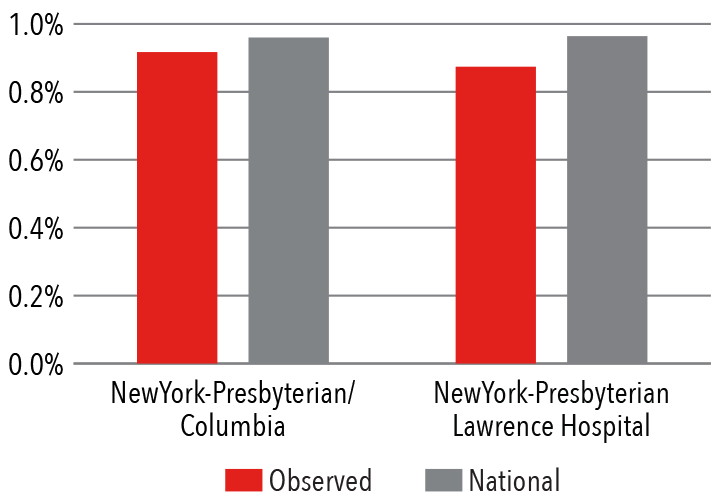
The Division of Hip and Knee Reconstruction performs more than 1,200 total, partial, and revision hip and knee replacements each year. Compared to the national average* for Medicare patients, NewYork-Presbyterian/Columbia's hip and knee surgeons demonstrate lower readmission rates and complications.
*Based on data from Premier, Inc.
Exploring Pain Management Modalities
In the last year, the orthopedics team explored new modalities and techniques in preemptive and postoperative pain control, particularly in knee replacement, through nerve blocks and combinations of medications. In the July 2018 issue of The Journal of Bone & Joint Surgery, they published the results of their study comparing the efficacy of adductor canal blocks (ACB) and periarticular anesthetic injections (PAI), both with bupivacaine, for pain management in total knee arthroplasty. This randomized controlled clinical trial demonstrated significantly higher pain scores and opioid consumption after total knee arthroplasty done with an ACB and without PAI, suggesting that ACB alone is inferior for perioperative pain control. Poster presentations on their pain management research were accepted by the American Association of Hip and Knee Surgeons and the American Academy of Orthopedic Surgeons.
Impact of Value-Based Care on Clinical Outcomes
The Division participates in the Comprehensive Care for Joint Replacement (CJR) Program, which aims to support better and more efficient care for Medicare beneficiaries undergoing hip and knee replacements. Initiated in 2016 by the Center for Medicare and Medicaid Services, this model tests bundled payment and quality measurement for an episode of care associated with hip and knee replacements to encourage hospitals, physicians, and post-acute care providers to work together to improve the quality and coordination of care from the initial hospitalization through 90 days postoperative recovery.
Cost-sharing revenue from CJR has been reinvested directly back into the clinical program, resulting in improved outcomes and a more positive patient experience for Medicare patients. Based on the success of the CJR program, the Division will be exploring other value-based opportunities with the goal of expanding the management of the 90-day episode of care for all orthopedic patients.
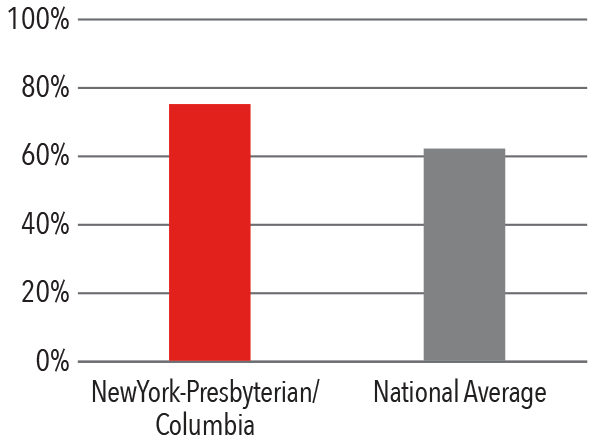
Enhancing Post-Discharge Care
Studies have shown that patients who meet certain discharge criteria related to physical, mental, and social factors recover better at home than at subacute rehabilitation facilities. By focusing on these aspects of postoperative care, Medicare patients undergoing surgery are discharged home more frequently than the national average. By improving relationships with local skilled nursing facilities and creating a network of subacute rehabilitation facilities, NewYork-Presbyterian/Columbia patients have a lower length-of-stay at rehabilitation facilities than the national average, resulting in improved outcomes, a lower infection risk, and higher patient satisfaction during the entire episode of care.
Patients Discharged Home Medicare
Average Number of Days in Subacute Rehabilitation Facility




