How and Why COVID-19 Targeted the Kidneys
As COVID-19 began to unfold in hospitals around the world, it quickly became clear that acute kidney problems were going to be among its major clinical manifestations. As the pandemic intensified in New York City to heights no one could imagine, Ali Gharavi, MD, Chief of Nephrology at NewYork-Presbyterian/Columbia University Irving Medical Center, and Manikkam Suthanthiran, MD, Chief of Nephrology and Hypertension at NewYork-Presbyterian/Weill Cornell Medical Center, and their teams quickly assimilated COVID-19 patients into their caseloads. At the same time, they identified strategies to address the gaps in resources as the number of patients needing intermittent dialysis and continuous renal replacement therapy continued to escalate, and kidney transplant recipients were being diagnosed with COVID-19 and requiring special attention.
With campuses located throughout New York City, NewYork-Presbyterian found itself at the epicenter of the pandemic. However, huge case volumes enabled nephrology faculty at NewYork-Presbyterian’s affiliated medical schools – Columbia University Vagelos College of Physicians and Surgeons and Weill Cornell Medicine – to bring their academic assets to bear on better understanding of the effects of COVID-19 on the kidneys. Following are highlights of several studies that clinician-researchers at Columbia and Weill Cornell pursued while simultaneously meeting the clinical demands of the increasing number of patients with COVID-19 and kidney dysfunction.
Quantifying the Impact
“We did expect to see COVID-19 patients with underlying kidney diseases knowing that those with diabetes and cardiovascular disease, kidney transplant recipients, patients with glomerular disease on immunosuppression, as well as individuals with end-stage kidney disease were among the more vulnerable,” says Dr. Ali Gharavi. “But at the beginning, reports from Europe and China did not sufficiently emphasize the potential for kidney failure. We essentially needed a disaster response to the COVID-19 surge in New York City.”
Dr. Ali Gharavi
To gauge the magnitude of the situation, Columbia researchers conducted a retrospective review of the first 1,000 patients presenting with COVID-19 at NewYork-Presbyterian/Columbia. Of these 1,000 patients, 150 came into the Emergency Department, 614 were admitted to the hospital, but not the ICU, and 236 were admitted or transferred to intensive care units. The review revealed that 33.9 percent of all patients with COVID-19 and 78 percent of patients in intensive care units developed acute kidney injury. This was a striking difference when compared with studies from China that reported 15 percent of all patients with COVID-19 developed acute kidney injury and a case series in Seattle that found 19.1 percent developed this condition.
At the same time, they found that 13.8 percent of all patients and 35.2 percent of patients in intensive care units required inpatient dialysis, leading to a shortage of equipment for dialysis and continuous renal replacement therapy. To guide the nephrology community, they also described the disaster response to the pandemic in New York City in a manuscript detailing the organization and allocation of resources for the inpatient and outpatient setting.
Read more:
Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, Bikdeli B, Ahluwalia N, Ausiello JC, Wan EY, Freedberg DE, Kirtane AJ, et al. Extrapulmonary manifestations of COVID-19. Nature Medicine. 2020 Jul;26(7):1017-1032.
The Division of Nephrology, Columbia University Vagelos College of Physicians and Surgeons Working Group. Disaster response to the COVID-19 pandemic for patients with kidney disease in New York City. Journal of the American Society of Nephrology. 31(7):1371-1379.
Characterizing and Caring for Kidney Disease in Relation to COVID-19
Dr. Manikkam Suthanthiran
“With acute kidney injury presenting as a life-threatening complication of COVID-19, it was imperative to determine the extent of kidney disease in these patients, identify the related clinical abnormalities, and understand the mechanisms underlying their development,” says Dr. Manikkam Suthanthiran. “The significant number of cases coming into the Weill Cornell Emergency Department provided us with an opportunity to begin uncovering patterns of kidney disease presentation and better understand the pathology, enabling us to optimize treatment and management.”
Acute Kidney Injury
To this end, Weill Cornell researchers from the Department of Nephrology and Hypertension, the Rogosin Institute, and the Department of Emergency Medicine conducted a retrospective cohort study of 1,002 patients admitted from March 1 to April 19, 2020, through the Emergency Department at NewYork-Presbyterian/Weill Cornell. Acute kidney injury (AKI) as defined by the Kidney Disease Improving Global Outcomes criteria occurred in 29 percent of the patients: 18 percent with stage one, 3 percent with stage two, and 8 percent with stage three. Of 294 patients, kidney replacement therapy was performed in 59 patients, 53 received hemodialysis and/or continuous venovenous hemodialysis, 5 received a combination of acute peritoneal dialysis and hemodialysis/continuous venovenous hemodialysis, and 1 patient received acute peritoneal dialysis.
The researchers uncovered several laboratory parameters that distinguished patients with and without AKI, including D-dimer levels, which were significantly higher in patients with AKI without kidney function recovery than in patients with AKI and kidney function recovery. The authors concluded that the high incidence of irreversible AKI in hospitalized patients with COVID-19 supports the importance of continued nephrology follow-up in these patients.
The unanticipated high incidence of AKI imposed extraordinary demands on the need for extracorporeal therapy. Innovations saved the day and every patient requiring dialysis support was treated with synergistic collaborations crossing divisions and departments. Acute peritoneal dialysis was reintroduced into the clinical arena with innovative surgeons placing the peritoneal dialysis catheter at the bedside and highly skilled nursing personnel providing invaluable technical assistance at NewYork-Presbyterian/Weill Cornell Medical Center. This interdisciplinary effort led by members of the Rogosin Institute and Nephrology faculty at Weill Cornell Medicine also led to the creation of a “how to” manual to facilitate widespread use of peritoneal dialysis as an effective alternative to continuous renal replacement therapy (CRRT) or hemodialysis.
“We observed that COVID-19 patients receiving CRRT experienced a higher than usual incidence of clotting. Refinement of anticoagulation strategies helped reduce clotting and prolonged filter life and improved the effectiveness of CRRT,” says Dr. Suthanthiran.
Read more:
Lee JR, Silberzweig J, Akchurin O, Choi ME, Srivatana V, Lin J, Liu F, Malha L, Lubetzky M, Dadhania DM, Shankaranarayanan D, Shimonov D, Neupane S, Salinas T, Bhasin A, Varma E, Leuprecht L, Gerardine S, Lamba P, Goyal P, Caliendo E, Tiase V, Sharma R, Park JC, Steel PAD, Suthanthiran M, Zhang Y. Characteristics of acute kidney injury in hospitalized COVID-19 patients in an urban academic medical center. Clinical Journal of the American Society of Nephrology. 2020 Sep 18:CJN.07440520. [Epub ahead of print]
Shankaranarayanan D, Neupane SP, Varma E, Shimonov D, Gerardine S, Bhasin A, Lamba P, Leuprecht L, Salinas T, Afaneh C, Bellorin-Marin OE, Srivatana V. Peritoneal dialysis for acute kidney injury during the COVID-19 pandemic in New York City. Kidney International Reports. 2020 Sep;5(9):1532-1534.
Shankaranarayanan D, Muthukumar T, Barbar T, Bhasin A, Gerardine S, Lamba P, Leuprecht L, Neupane SP, Salinas T, Shimonov D, Varma E, Liu F. Anticoagulation strategies and filter life in COVID-19 patients receiving continuous renal replacement therapy: A single-center experience. Clinical Journal of the American Society of Nephrology. 2020 Sep 17: CJN.08430520. [Epub ahead of print]
End-Stage Kidney Disease
The risk of COVID-19, particularly severe disease in patients with end-stage kidney disease (ESKD), given their immunocompromised state and high burden of comorbidities, was uncertain. Analyses by researchers in Columbia’s Department of Nephrology of presentation and outcomes of COVID-19 in 59 patients with ESKD on dialysis was among the first to demonstrate the high mortality rate in this patient population.
The authors note that “although the presentation of patients on dialysis with COVID-19 was similar to that of the general population, these patients have poor outcomes, including 31 percent overall mortality and 75 percent mortality among those requiring mechanical ventilation. The high mortality rates in patients with ESKD on dialysis reinforced the need to take appropriate infection control measures to prevent COVID-19 spread in this vulnerable population.”
Read more:
Valeri AM, Robbins-Juarez SY, Stevens JS, Ahn W, Rao MK, Radhakrishnan J, Gharavi AG, Mohan S, Husain SA. Presentation and outcomes of patients with ESKD and COVID-19. Journal of the American Society of Nephrology. 2020 Jul;31(7):1409-15.
Positively Impacting Care
Whereas the initial focus was on ventilator shortage in patients with COVID-19 and respiratory failure, it soon became apparent that dialysis support was a much needed and lifesaving procedure in this patient population. The unprecedented demand for extracorporeal therapy was reminiscent of the early days of dialysis in the 1960s when decisions were made regarding who is eligible for dialysis.
A thoughtful perspective from a distinguished group of nephrologists (with nephrology faculty from the Rogosin Institute and Weill Cornell Medicine as the lead authors), published in the Journal of American Society of Nephrology, enunciated considerations for a broad group of stakeholders and laid the groundwork for managing future pandemics. As a complementary and much needed piece, guidelines for mitigating risk of COVID-19 in dialysis facilities was published as well.
Read more:
Silberzweig J, Ikizler TA, Kramer H, Palevsky PM, Vassalotti J, Kliger AS. Rationing scarce resources: The potential impact of COVID-19 on patients with chronic kidney disease. Journal of the American Society of Nephrology. 2020 Sep;31(9):1926-1928.
Kliger AS, Silberzweig J. Mitigating risk of COVID-19 in dialysis facilities. Clinical Journal of the American Society of Nephrology. May 2020.15(5)707-709.
Mechanism of Pathology
Understanding the mechanism of kidney injury among patients with COVID-19 remains an urgent need in order to be able to manage this complication successfully. As an important step towards understanding the patterns of injury, Columbia researchers evaluated biopsy samples of native and allograft kidneys from 17 patients with COVID-19 between March and June 2020.
While each of the patients presented with at least one comorbidity, none had known preexisting lung disease. The biopsy series, which comprised 14 native and three allograft kidneys, revealed a diversity of glomerular and tubular diseases and provided evidence against direct viral infection of the kidneys as the major pathomechanism for COVID-19-related kidney injury and, instead, implicated cytokine-mediated effects and heightened adaptive immune responses.
In an autopsy study performed by Columbia nephrologists and pathologists, the predominant kidney lesion was acute tubular injury. Interestingly, none of the samples tested showed positivity for the SARS-Cov-2 virus by in-situ hybridization.
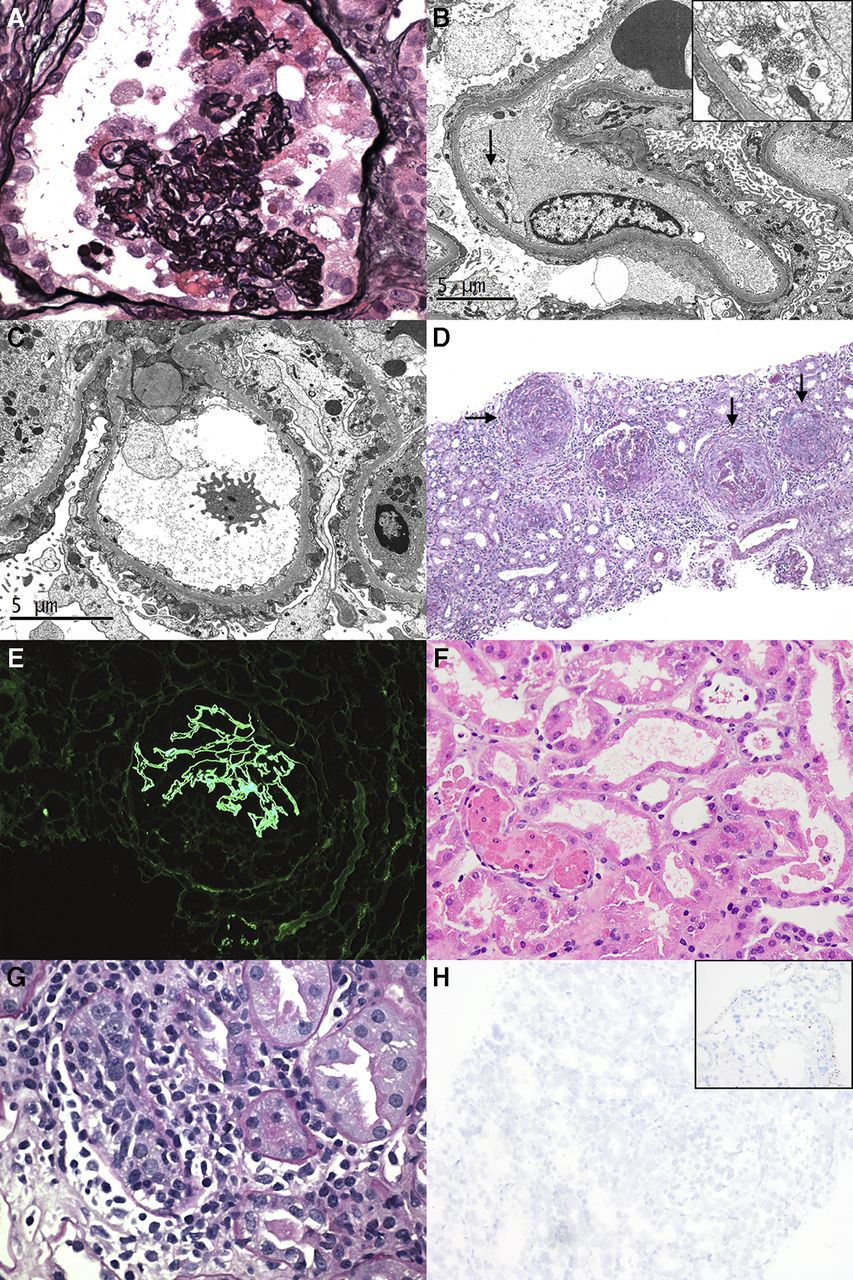
Kidney biopsy findings in patients with COVID-19 (A) Light microscopy demonstrates a lesion of collapsing glomerulopathy (B) Diffuse foot process effacement and endothelial TRIs (arrow and inset) in a patient with minimal change disease (C) Subepithelial electron dense deposits in PLA2R-associated membranous glomerulopathy (D) Multiple glomeruli with circumferential cellular crescents (arrows) in a patient with class 4+5 lupus nephritis (E) A glomerulus compressed by a crescent with global linear GBM staining for IgG in a patient with anti-GBM nephritis (F) Tubular simplification and focal shedding of degenerating epithelial cells into the tubular lumina in a patient with isolated ATI (G) Severe lymphocytic tubulitis in a patient with acute T cell-mediated rejection (H) ISH for the virus by automated method showing undetectable viral RNA in the kidney; inset shows positive lung control (Courtesy of Columbia University Irving Medical Center)
Read more:
Kudose S, Batal I, Santoriello D, Xu K, Barasch J, Peleg Y, Canetta P, Ratner LE, Marasa M, Gharavi AG, Stokes MB, Markowitz GS, D’Agati VD. Kidney biopsy findings in patients with COVID-19. Journal of the American Society of Nephrology. 2020 Sep;31(9):1959-68.
Santoriello D, Khairallah P, Bomback AS, Xu K, Kudose S, Batal I, Barasch J, Radhakrishnan J, D’Agati V, Markowitz G. Postmortem kidney pathology findings in patients with COVID-19. Journal of the American Society of Nephrology. 2020 Sep;31(9):2158-2167.
Tremendous Value of Telehealth
The dialysis population is at high risk for infection with SARS-CoV-2; the mortality rate is also higher in patients requiring dialysis support because of co-existing morbidities such as diabetes and hypertension. Telehealth served as a powerful platform enabling ongoing monitoring of patients dialyzed at home while reducing infection exposure. The remote monitoring was spearheaded by members of the Rogosin Institute and Nephrology faculty at Weill Cornell Medicine. The positive experience gained by remote monitoring of home dialysis patients is likely to serve as the stimulus to expand the use of remote monitoring to a broader group of patients with kidney disease.
Read more:
Srivatana V, Liu F, Levine DM, Kalloo SD. Early use of telehealth in home dialysis during the COVID-19 pandemic in New York City. Kidney360. 1(6)524–526, 2020.
Lew SQ, Wallace EL, Srivatana V, Warady BA, Watnick S, Hood J, White DL, Aggarwal V, Wilkie C, Naljayan MV, Gellens M, Perl J, Schreiber MJ. Telehealth for home dialysis in COVID-19 and beyond: A perspective from the American Society of Nephrology COVID-19 Home Dialysis Subcommittee. American Journal of Kidney Diseases. 2020 Sep 28:S0272-6386(20)31004-0. [Epub ahead of print]
Unique Vulnerabilities of Transplant Patients
From the outset of the pandemic there was particular concern for recipients of solid organ transplants given their suppressed immune systems. While the impact of chronic immunosuppression on outcomes of COVID-19 was not known, it was potentially very relevant since host inflammatory responses appeared to constitute an important cause of associated organ injury. In addition, it was expected that high rates of comorbidities, frequent contact with medical care, and chronic immunosuppression among solid organ transplant recipients would put them at high risk of infection and poor outcomes.
The Broad View
Columbia and Weill Cornell researchers prospectively collected data on these patients, including clinical characteristics, features at presentation, and the clinical management, including antiviral and immunosuppressive therapy between those patients with mild/moderate disease and those with severe disease (ICU admission, intubation, or death). Of the 90 patients analyzed, 46 were kidney, 17 lung, 13 liver, 9 heart, and 5 dual-organ transplant recipients. There were 68 patients hospitalized, and findings suggested that transplant recipients with COVID-19 appeared to have more severe infections and worse outcomes overall: 12 percent required non-rebreather and 35 percent required intubation. Sixteen patients died (18 percent overall, 24 percent of hospitalized, 52 percent of ICU) and 37 patients (54 percent) were discharged. There was no clear difference between disease severity and type of organ transplant in this cohort, and patients who progressed to severe disease were often already hypoxic and tachypneic on presentation.
As investigators the world over continue to clarify the mechanisms of and therapeutic strategies for COVID-19, transplant specialists at NewYork-Presbyterian persevere in their investigations to determine the role of the immune response in order to guide appropriate immunomodulatory therapy, which may differ among the various solid organ transplant recipients.
Read more:
Pereira MR, Mohan S, Cohen DJ, Husain SA, Dube GK, Ratner LE, Arcasoy S, Aversa MM, Benvenuto LJ, Dadhania DM, Kapur S, Dove LM, Brown RS Jr, Rosenblatt RE, Samstein B, Uriel N, Farr MA, Satlin M, Small CB, Walsh TJ, Kodiyanplakkal RP, Miko BA, Aaron JG, Tsapepas DS, Emond JC, Verna EC. COVID-19 in solid organ transplant recipients: Initial report from the U.S. epicenter. American Journal of Transplantation. 2020 Apr 24. [Epub ahead of print]
A Focus on Kidney Transplant – Early Days
With a high volume of patients and major kidney transplant programs, the Division of Nephrology at Columbia University and the Division of Nephrology and Hypertension and Department of Transplantation Medicine at Weill Cornell Medicine collected data prospectively from their respective kidney transplant patients to shed light on what they could expect going forward and optimize management when their patients presented with COVID-19.
Faculty in the Columbia University Kidney Transplant Program examined a series of 15 consecutive kidney transplant recipients who required hospitalization through March 27, 2020, representing one of the earliest series of its kind – meeting an urgent need to understand what to expect among these patients. The authors note that overall presenting symptoms of COVID-19 in kidney transplant was similar to that reported for the general population but the absence of abnormal chest X-rays in over a third of patients was a key insightful finding.
Approximately a quarter of patients eventually required mechanical ventilator support and 2 patients died eventually – a mortality rate lower than that was reported in other cohorts. Researchers were also the first to note the association of infections with the use of immunosuppressive regimens that included low dose prednisone – a finding that has since been replicated in other cohorts. While many of their patients experienced a favorable outcome with the current treatment strategy, including immunosuppression reduction, longer-term studies would be needed going forward.
Read more:
Columbia University Kidney Transplant Program. Early description of coronavirus 2019 disease in kidney transplant recipients in New York. Journal of the American Society of Nephrology. 2020 Apr 21. [Epub ahead of print]
Optimizing Survival
In a pivotal study of 73 consecutive adult kidney graft recipients with suspected COVID-19 from March 20 to April 20, Nephrology and Transplantation Medicine faculty at Weill Cornell Medicine, in collaboration with their colleagues in internal medicine, infectious disease, and transplantation surgery, demonstrated that an effective, systematic strategy for evaluation and triage of patients to ambulatory care or hospitalization combined with judicious management of immunosuppressive drug therapy resulted in excellent outcomes in kidney transplant recipients diagnosed with COVID-19.
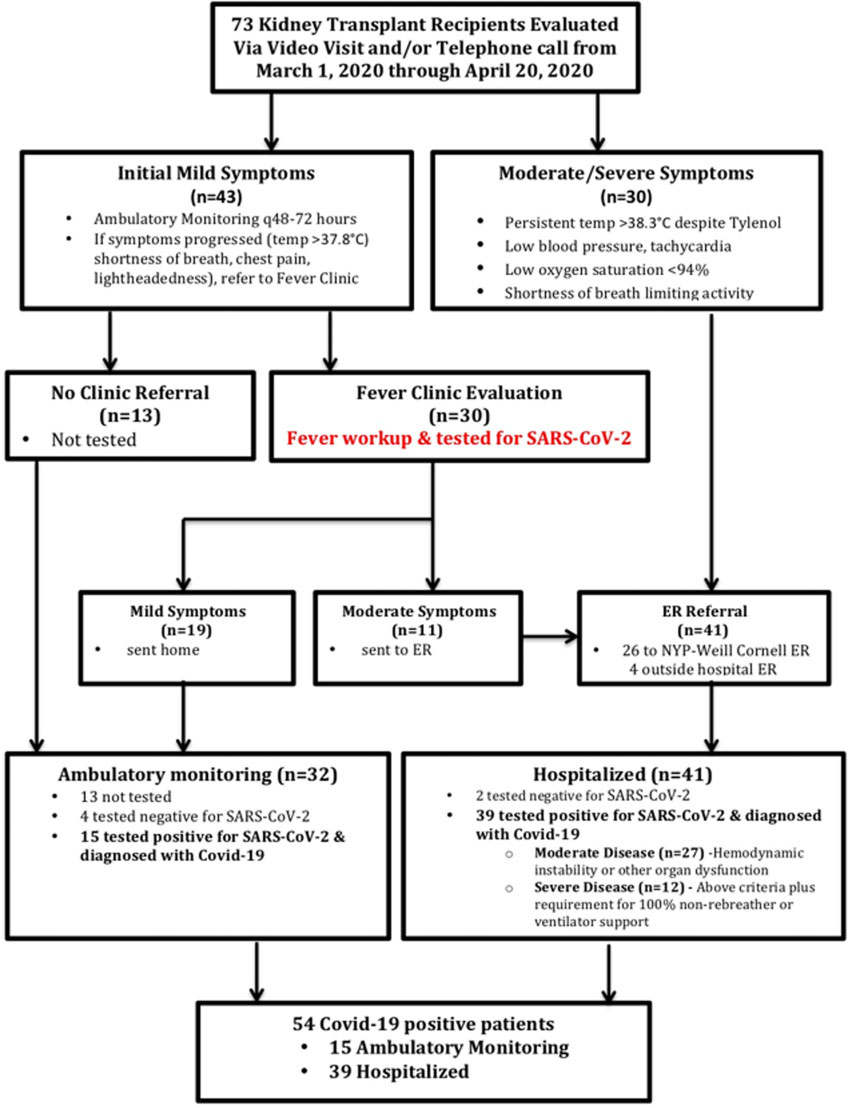
As illustrated in the flowchart, the integrated approach involved telephone calls, video visits, and referrals to the Fever Clinic and Emergency Department at Weill Cornell depending upon the severity of the symptomatology. Of the 73 adult kidney graft recipients suspected of COVID-19, 54 tested positive for SARS-CoV-2 by RT-PCR test. Among these 54 patients, 39 had moderate to severe symptoms and required hospitalization, and 15 had mild symptoms and were managed in the ambulatory setting with close monitoring by the kidney transplant team. The figure below shows the weekly cases during the early days of the COVID-19 pandemic.
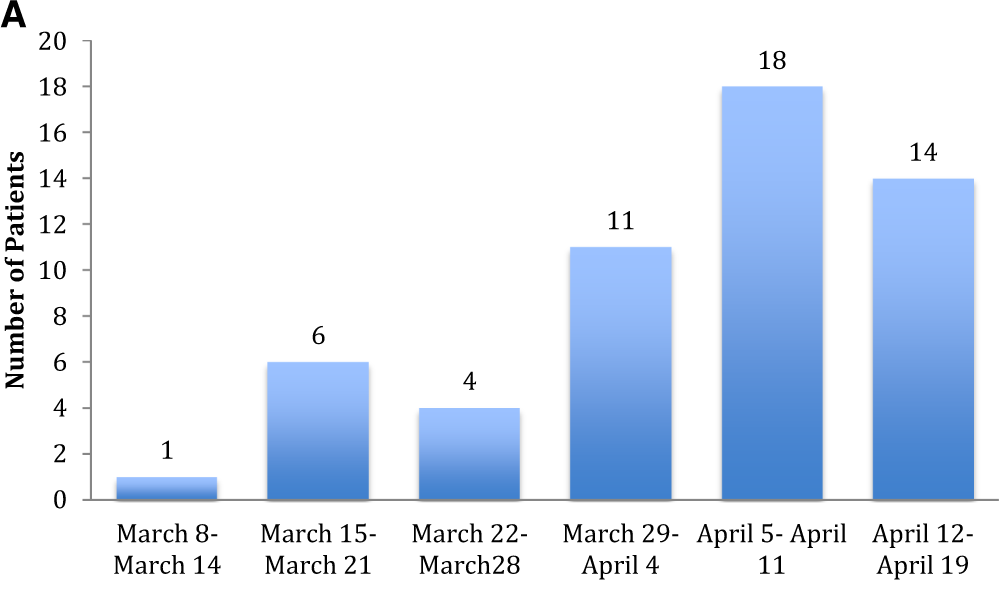
(A) Number of kidney transplant recipients from the Weill Cornell transplant center who received a diagnosis of COVID-19 for each week during the study period
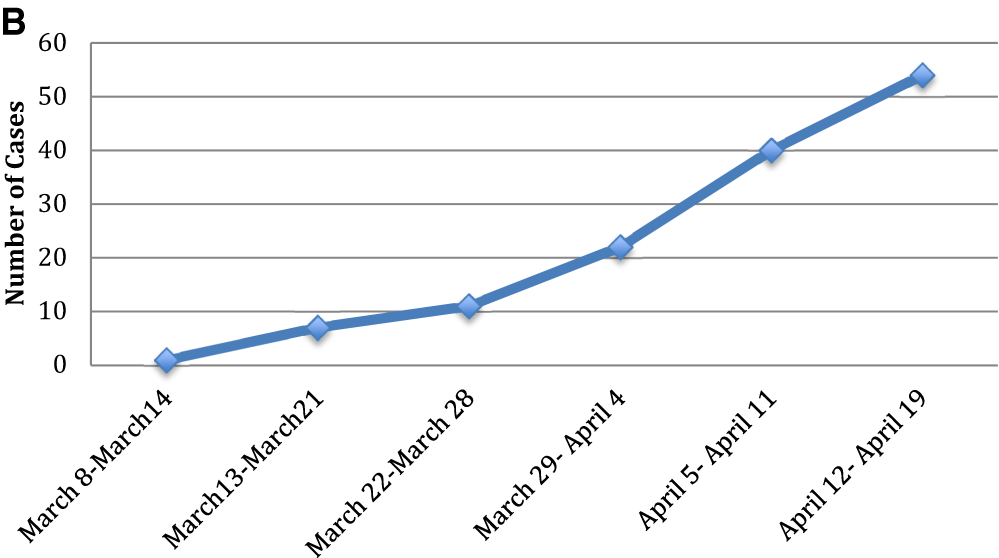
(B) Cumulative cases of kidney transplant recipients with COVID-19 for each week during the study period (Lubetzky M et al. Nephrology Dialysis Transplantation 2020)
At this juncture, very little data was available on how to treat these high-risk transplant patients. Early in the pandemic there was some consensus within the transplant community to reduce or withhold immunosuppression, and the team had two critical questions to address: Is it possible that immunosuppressive agents may, in fact, provide protective effects against COVID-19? Is the cytokine storm associated with this virus a contributor to acute respiratory distress syndrome more or less likely to occur in patients who are on immunosuppressive therapy, which is known to inhibit cytokine release?
Based on mechanisms of action of immunosuppressive drugs prescribed for kidney transplant recipients and based on the Weill Cornell Medicine team’s findings that the cytokines implicated in the cytokine storm associated with COVID-19 are blocked by the very same immunosuppressive drugs including steroids, the transplant team chose to continue immunosuppressive drugs rather than discontinue immunosuppressive therapy and implemented a personalized approach to immunosuppressive therapy. In the 15 kidney transplant recipients with COVID-19 managed in the ambulatory setting, the dosage of the primary immunosuppressive drug, tacrolimus, was maintained. Steroids were continued in all 6 patients receiving maintenance steroid therapy and the dose of mycophenolate mofetil was reduced by 50 percent in 5 of 15 (33 percent) patients.
In the 39 patients requiring hospitalization, individualization of immunosuppressive drug therapy consisted of a modest reduction in tacrolimus dosage in 54 percent and continuation of steroid therapy in all 16 patients (41 precent) on maintenance steroids. As of May 15, 2020, approximately 37 days after infection, the overall survival was 87 percent in the total cohort of 54 patients and 82 percent in the 39 hospitalized patients. The observed survival rates compare very favorably with the published data. Viewed through the lens of a recent landmark study that steroids reduce mortality in COVID-19 patients, our strategy of continuing immunosuppressive drug therapy, including steroids, may have contributed to excellent patient survival in our kidney allograft recipients diagnosed with COVID-19.
Mortality Rate in Kidney Graft Recipients Diagnosed with COVID-19
The percentage of death was 32 percent in the 144 patients from the TRANGO International Transplant Consortium (Cravedi P et al. American Journal of Transplantation 2020); 28 percent in the 36 consecutive kidney graft recipients from a non-NewYork-Presbyterian transplant center (Akalin E et al. The New England Journal of Medicine 2020); and 13 percent in the 54 consecutive patients transplanted at NewYork-Presbyterian/Weill Cornell (Lubetzky M et al. Nephrology Dialysis Transplantation 2020)
Read more:
Lubetzky M, Aull MJ, Craig-Schapiro R, Lee JR, Marku-Podvorica J, Salinas T, Gingras L, Lee JB, Sultan S, Kodiyanplakkal RP, Hartono C, Saal S, Muthukumar T, Kapur S, Suthanthiran M, Dadhania DM. Kidney allograft recipients, immunosuppression, and coronavirus disease-2019: A report of consecutive cases from a New York City transplant center. Nephrology Dialysis Transplantation. 2020 Jul 1;35(7):1250-61.
To Transplant or Not to Transplant During the COVID-19 Pandemic
The Weill Cornell Medicine team has begun to address the critical question of whether it was safer for patients to remain on the kidney transplant waitlist or proceed with kidney transplantation during the COVID-19 pandemic. The team compared the outcomes of 56 waitlisted patients positive for SARS-CoV-2 with the outcomes of 80 kidney transplant recipients positive for SARS-CoV-2 between March 13 and May 20, 2020. The demographics and the burden of comorbidities were not significantly different between the two groups. However, the rate of hospitalization for the waitlisted patients was significantly higher compared to the kidney transplant cohort: 82 percent vs. 65 percent, respectively (P=0.03). The case fatality rate was significantly higher in the waitlisted cohort compared to the kidney transplant cohort, 34 percent vs. 16 percent, respectively (P=0.02).
As observed in the general COVID-19 population, there was a preponderance of male sex in those who died – 84 percent in the waitlist group and 100 percent in the kidney transplant group. Statistical analysis identified that waitlist status, age, and male sex are independently associated with mortality. Our findings have significant implication for managing patients waitlisted for kidney transplants and raise the intriguing possibility that transplantation may be the safer option despite the risks of exposure to COVID-19. This transplant option requires careful screening of recipients and identification of appropriate donors and personalized immunosuppressive drug regimen.
Read more:
Craig-Schapiro R, Salinas T, Lubetzky M, Abel BT, Sultan S, Lee JR, Kapur S, Aull MJ, Dadhania DM. COVID-19 outcomes in patients waitlisted for kidney transplantation and kidney transplant recipients. American Journal of Transplantation. 2020 Oct 12. [Epub ahead of print]
COVID-19 and Hypertension
A finding of considerable clinical significance was the discovery that SARS-CoV-2 gains entry into the cell following binding to the cell surface receptor called ACE2, an enzyme that is involved in the generation of vasoactive peptides that are part of the renin angiotensin system (RAS). Given that at least 50 percent of the millions of individuals with hypertension and kidney disease are treated with blockers of the RAS, such as angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARB), there was a tremendous concern among physicians and patients whether the RAS blockers used to treat hypertension may promote viral entry and increase SARS-CoV-2 infection rate or worsen COVID-19.
Because stoppage of RAS blockers would have adverse outcomes in itself, our Hypertension team conducted an analysis of existing literature and concluded that on balance it was safer to continue RAS blocker therapy than stopping these highly effective anti-hypertensive drugs. Their recommendation to continue with RAS blockade therapy was also informed by the consideration that blocking angiotensin II may, in fact, be beneficial in preventing severe lung damage due to COVID-19. The team’s reasoned conclusions, published in March 2020, have received strong support from subsequent reports that continuation of RAS blockade is safe in patients at risk for COVID-19 and patients diagnosed with COVID-19. Angiotensin converting enzyme inhibitors and angiotensin receptor blockers are not being withheld in patients at risk for COVID-19 or diagnosed with COVID-19.
Read more:
Malha L, Mueller FB, Pecker MS, Mann SJ, August P, Feig PU. COVID-19 and the renin-angiotensin system. Kidney International Reports. 2020 Mar 27;5(5):563-565.
“It has been said that adversity builds character. What I witnessed was adversity revealing the true character of the highly dedicated individuals unflinchingly taking on the physical and emotional challenges of managing COVID-19 patients,” says Dr. Suthanthiran. “It was a team effort in every sense of the term with each contributing their individual best. I am personally grateful to our fellows and faculty, our cross-campus collaboration with Dr. Gharavi and his team at Columbia, and the NewYork-Presbyterian/Weill Cornell staff and its inspired leadership for their efforts to help us realize the promise of academic medicine – creating and translating new knowledge for the betterment of our patients.”