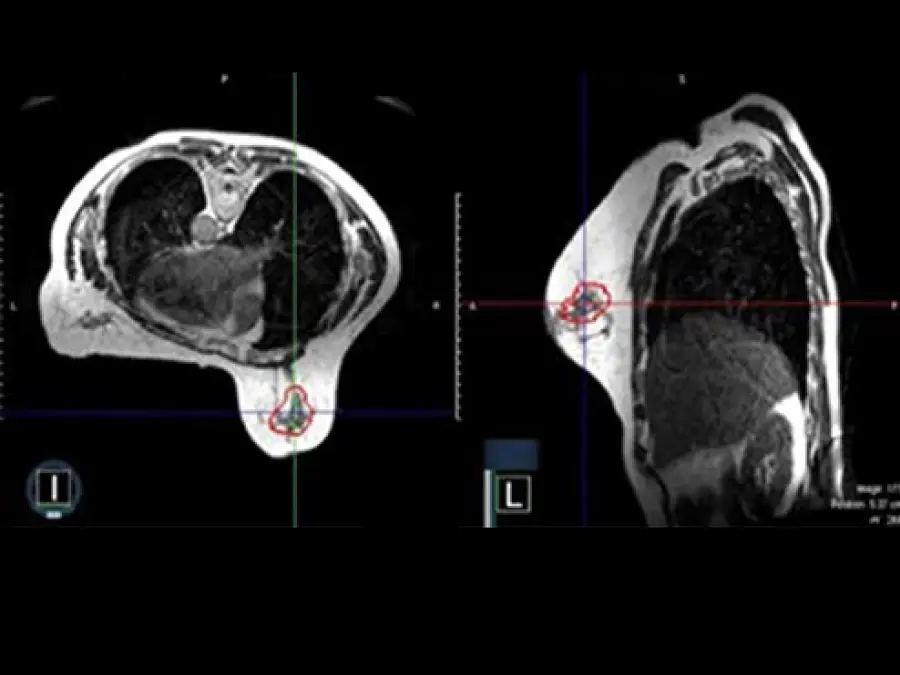
Phosphoinositide 3-kinase (PI3K) is one of the most mutated proteins in breast and other cancers. NewYork-Presbyterian/ Columbia’s Dr. Neil Vasan has dedicated his career to studying PI3K mutations and their role in predicting response to treatment. In his latest research, Dr. Vasan found that women whose breast cancers harbored double mutations responded better to PI3K inhibitors, a finding that’s now being investigated further in multiple clinical trials. Last year, Dr. Vasan was one of 58 investigators in the country to receive a prestigious New Innovator Award from the National Institutes of Health’s High-Risk, High- Reward program. This award will help extend his work on the PI3K kinase to all 556 kinase genes in the human genome, in hopes of determining the consequences to cancer cells of turning off kinase enzymes, which has immense potential to transform our understanding of kinases and kinase inhibitors.