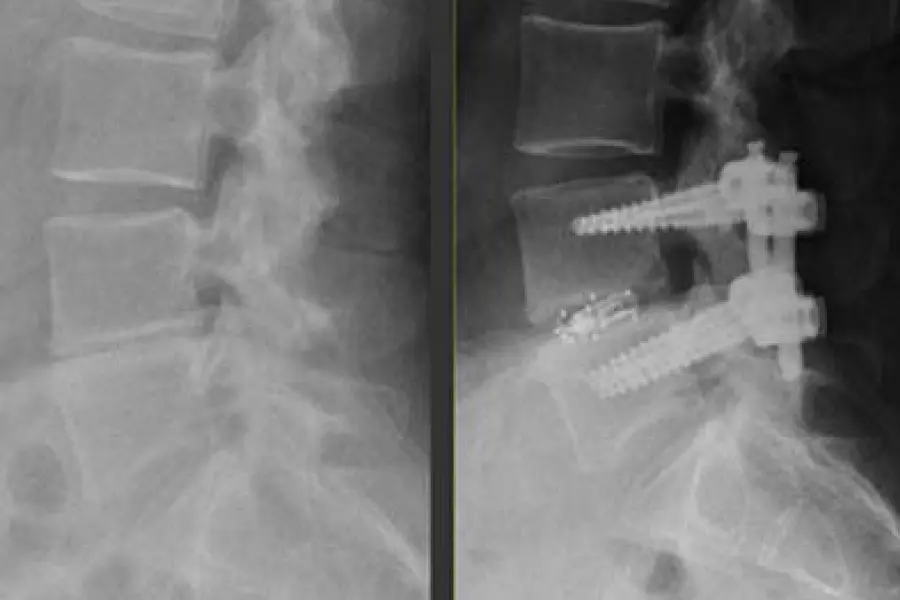
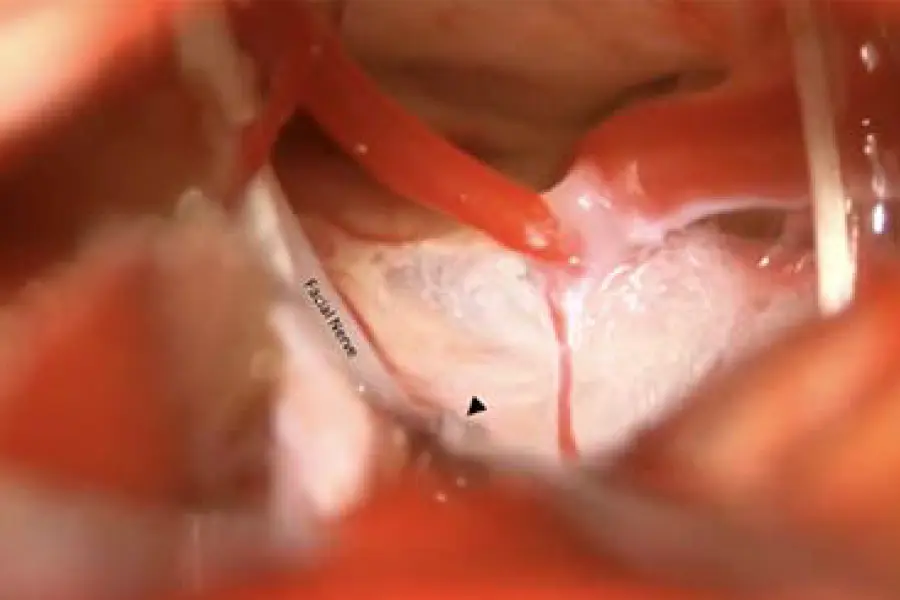
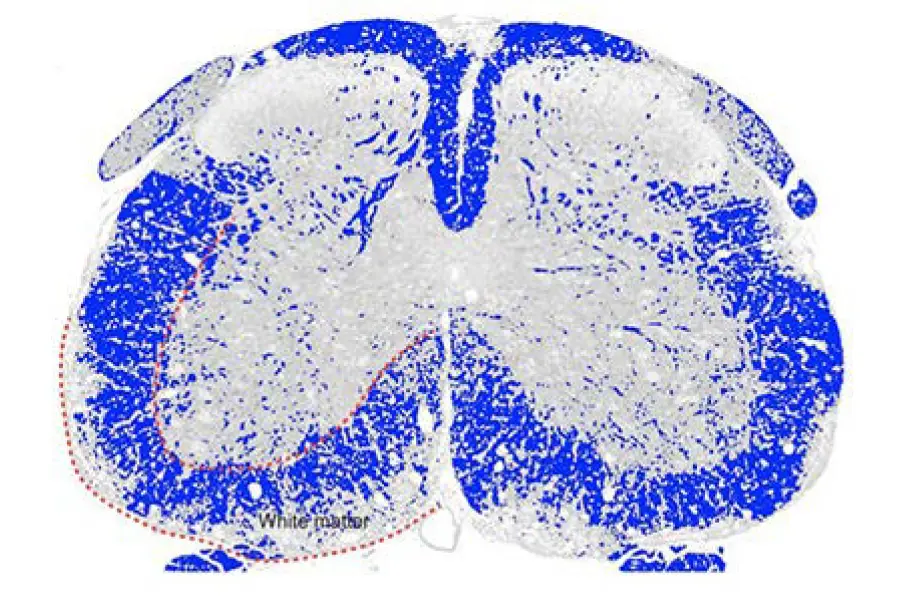
Dr. Ibrahim Hussain, a neurological spine surgeon at Och Spine at NewYork-Presbyterian, performed the first 3D-navigation-guided endoscopic transforaminal lumbar interbody fusion (TLIF) in New York City. This innovative procedure for treating lumbar degenerative pathologies relies on 3D navigation to map a trajectory that avoids nerve injury and helps customize the size of the implant. A collapsed interbody “cage” is expanded after placement inside the disc space under endoscopic visualization. In contrast to open TLIF and minimally invasive TLIF, 3D endoscopic TLIF requires a smaller incision, minimal bone and muscle dissection, and less sedation, resulting in a faster and less painful recovery.