What are Left Ventricular Assist Devices (LVADs)?
What is a Left Ventricular Assist Device (LVAD)?A left ventricular assist device (LVAD) is a small, surgically implanted mechanical pump that supports a weakened heart's left ventricle. When the left pumping chamber of the heart thickens — known as left ventricular hypertrophy — it may not be able to pump efficiently. LVADs help ensure the heart pumps enough blood to meet the body's needs.
An LVAD can provide lifesaving support for people dealing with a variety of life-threatening conditions and help improve their overall quality of life. These devices are often used in patients with advanced heart failure.
NewYork-Presbyterian has more than 30 years of experience in LVAD implantation and monitoring. Our internationally known experts have pioneered innovation and technological progress in this field. We specialize in managing complex cases, often treating patients deemed too ill to receive an LVAD by other institutions.
How Does an LVAD Work?
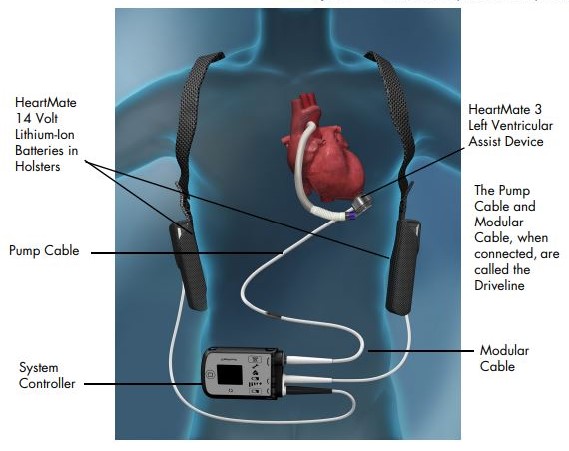
How Does it Work?An LVAD pump and its connections are implanted next to the heart during open-heart surgery. One end of the pump is attached to the left ventricle — the heart chamber that pumps blood and distributes it throughout the body.
The other end is attached to the aorta — the body's main artery. Blood flows from the heart into the pump. When sensors indicate that the LVAD is full, the blood in the device is distributed into the aorta. The aorta then distributes blood to the rest of the body.
In addition to the pump, the other components of the LVAD include a flexible tube called a driveline. The driveline connects through the skin to a small external computer called a controller which is battery-powered. (Both the controller and power source are worn outside the body, often using a special belt or harness around the waist or stomach.)
Over the past three decades, doctors have made tremendous improvements in LVAD therapy — progressing from bulky, noisy pumps with limited durability (typically lasting one to two years) to smaller, silent, more durable pumps.
How Are LVADs Used?
How are They Used?Your doctor will let you know if you could benefit from LVAD therapy. In many cases, left ventricular assist devices can increase a left ventricular hypertrophy patient’s life expectancy. The risks and benefits will be carefully discussed, and the decision to proceed will be based on your personal history and preferences. LVADs can be beneficial for:
Advanced heart failure
People with advanced heart failure may need an LVAD when medications and other treatments are no longer effective. An LVAD can reduce heart failure symptoms such as shortness of breath, fatigue, leg swelling, diminished exercise capacity, and problems with liver and/or kidney function. It may also reduce recurrent hospital admissions due to heart failure.
Bridge to heart transplant (BTT)
Waiting for a heart transplant can take weeks, months, or even years. LVAD implantation helps support heart function, so a patient's condition does not worsen while waiting for a transplant. This can help prevent damage to other organs, including the lungs, liver, and kidney while improving quality of life. Once a donor's heart is transplanted, the LVAD is removed.
Bridge to decision
In cases where patients have advanced organ failure caused by heart failure, and are therefore ineligible for an immediate heart transplant, an LVAD can be used to help stabilize organ failure. They may still be eligible for a heart transplant in the future.
Bridge to recovery
Some patients may benefit from LVAD if their heart is expected to recover its function but may not do so with medications alone. This may be the case with heart failure that develops after cardiac surgery, inflammation of the heart that is expected to improve, or heart failure that develops after having a baby.
Destination therapy (DT)
If a patient is not a candidate for heart transplantation due to age or other factors, an LVAD can prolong and improve their life. In these cases, as opposed to serving as a "bridge" to a heart transplant, the LAVD serves as the "destination" itself, with the device in use for the remainder of the patient's life. Destination therapy is often used to treat severe heart failure in patients who are not candidates for a transplant.
At NewYork-Presbyterian, we have developed a state-of-the-art protocol to give our patients the best chance of recovery. If heart function does improve, doctors will begin the appropriate testing to see if the LVAD can be removed safely.
What Conditions Does LVAD Treat?
Conditions TreatedLeft ventricular assist devices are primarily used to treat advanced heart failure. Advanced heart failure is a chronic, progressive condition that occurs when the heart is unable to pump enough oxygen-rich blood throughout the body. This is heart failure in its most serious stage — also known as stage D.
The heart may become enlarged as it works harder and faster to pump more blood. This can result in fatigue, weight gain, shortness of breath, a bloated or hard stomach, loss of appetite or nausea, and a dry, hacking cough. There may also be swelling in the legs, ankles, and abdomen. Heart failure can cause damage to other organs and result in fluid buildup in the lungs.
Risks to Consider
RisksBecause there are several risks and complications associated with LVADs, patients require anticoagulation and antiplatelet agents after LVAD surgery to reduce the risk of blood clots. LVAD complications can occur both early on (less than 30 days after placement) or later (more than 30 days after placement).
Risks and complications of LVAD implantation include:
- Infection
- Internal bleeding
- Blood clots and/or stroke
- Device malfunction
- Kidney failure
- Respiratory failure
- Heart failure
Contact Us
Call for an Appointment
NewYork-Presbyterian/Columbia University Irving Medical Center ‒ Milstein Family Heart Center
Heart Failure & Transplantation Program
NewYork-Presbyterian/Weill Cornell Medical Center ‒ Ronald O. Perelman Heart Institute
Heart Failure Program