What is Cervical Cancer?
What is Cervical Cancer?Cervical cancer is cancer that affects the cervix. Cancer occurs when cells in the body replicate uncontrollably, leading to tumors and possible damage to healthy tissue. It can begin anywhere and can spread to different locations in the body. Cervical cancer starts in the cells of the cervix.
Cervical cancer was once a leading cause of death for women in the United States, but it has become much less common in recent years due to screening tests such as the Pap test and the introduction of the HPV vaccine.
What is the cervix?
The cervix is the lower part of the uterus. It connects the main body of the uterus to the vagina (birth canal). During pregnancy, a fetus grows and develops in the uterus, and during childbirth, the cervix dilates to allow the baby to pass through the birth canal and out of the body.
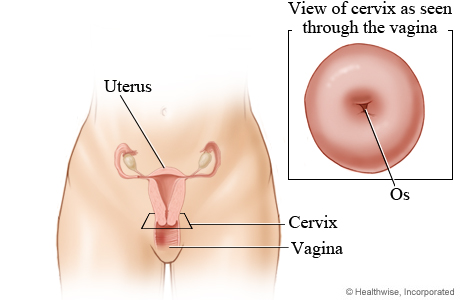
The cervix is made up of two different parts: the endocervix and the exocervix. The endocervix is the inner part of the cervix that leads into the uterus. It is lined with glandular cells, which are tall and column-shaped. The exocervix is the outer part of the cervix that extends into the vagina. It is lined with squamous cells, which are flat and thin. Different types of cervical cancer are determined by the type of cell that the cancer affects.
Stages of Cervical Cancer
StagesThe stages of cervical cancer are broken down into four primary stages, each with sub-stages indicating more specific characteristics regarding the progression of cancer:
- Stage 1 - Cancer remains confined to the cervix and has not spread beyond the cervix to other body parts
- Stage 1A - Cervical cancer is very small and has been detected and diagnosed through the observation of cell samples under a microscope
- 1A1 - The cancerous area is less than 3 mm in depth
- 1A2 - The cancerous area is between 3 mm and 5 mm in depth
- Stage 1B - The cancer has grown larger but is still only within the cervix
- 1B1 - The tumor is now 5 mm or greater in-depth and less than 2 cm wide
- 1B2 - The tumor is 5 mm or greater in depth and measures between 2 and 4 cm wide
- 1B3 - The tumor is now 4 cm or greater in width
- Stage 1A - Cervical cancer is very small and has been detected and diagnosed through the observation of cell samples under a microscope
- Stage 2 - Cancer has spread beyond the cervix/uterus to tissues adjacent to the cervix. It is still confined to the pelvic area and has not spread to nearby lymph nodes or other body parts.
- 2A –Cancer has spread to the upper vagina. However, it is still not found in the lower part of the vagina or the tissue surrounding the cervix known as the parametria.
- 2A1 - The tumor measures less than 4 cm
- 2A2 - The tumor measures 4 cm or greater
- 2B - Cancer has spread to the parametria
- 2A –Cancer has spread to the upper vagina. However, it is still not found in the lower part of the vagina or the tissue surrounding the cervix known as the parametria.
- Stage 3 - Cancer has spread to the lower part of the vagina and possibly the pelvic wall. It is also possible that it has spread to neighboring lymph nodes, but has not yet spread to other more distant parts of the body.
- 3A - Cancer has spread to the lower vagina but does not involve the pelvic sidewall
- 3B - Cancer involves the pelvic sidewall and may impact proper kidney function. This is known as hydronephrosis, which involves upstream swelling in one or both kidneys due to downstream drainage obstruction by a tumor.
- 3C - This stage involves the spread of cancer to the lymph nodes
- 3C1 - Cancer has spread to the nearby pelvic lymph nodes
- 3C2 - Cancer has spread to the para-aortic lymph nodes located in the abdomen along the aorta (a major artery)
- Stage 4 - Cancer has now spread to nearby pelvic organs and/or more distant parts of the body
- 4A - Cancer has grown and now directly invades adjacent pelvic organs such as the rectum or bladder
- 4B - Cancer has now spread beyond the pelvis to distant areas of the body such as the lungs, liver, or other more distant lymph nodes
Types of Cervical Cancer
TypesThe main types of cervical cancer are:
- Squamous cell carcinoma - Develops in squamous cells of the exocervix. This is the most common type of cervical cancer, accounting for almost 90% of cervical cancer diagnoses.
- Adenocarcinoma - Affects glandular cells of the endocervix
- Adenosquamous carcinoma - Less common and affects both glandular and squamous cells
- Rarely, cervical cancer can affect other cells in the cervix, leading to other types of cancer, including sarcoma, lymphoma, or melanoma. However, these cancers are more common in other parts of the body.
Signs & Symptoms of Cervical Cancer
SymptomsIn its early stages, cervical cancer often does not produce symptoms. This makes regular screenings crucial for detecting cancer early, possibly even before cervical cancer symptoms are experienced, so that treatment can begin promptly.
Common symptoms of Stage I cervical cancer include:
- Abnormal vaginal bleeding after sex, between periods, or after menopause
- Bloody or watery vaginal discharge that may have a strong odor
- Pelvic pain
- Pain during sex
Other common signs and symptoms of more advanced cervical cancer are:
- Difficulty urinating
- Blood in urine
- Changes in bowel movements, which may include diarrhea or bloody stool
- Swelling of the legs
- General feelings of illness, such as fatigue or loss of appetite
Cervical cancer can metastasize or spread to other areas of the body, which may cause additional symptoms in those locations. Learn more about metastatic cancer here.
Causes & Risk Factors of Cervical Cancer
Causes & Risk FactorsCervical cancer occurs when mutations in cells of the cervix cause them to grow and multiply uncontrollably. Certain factors can increase the likelihood of this abnormal cell growth, including:
- Infection with HPV (human papillomavirus) – The most common cause of cervical cancer
- Sexual history - A woman’s risk of cervical cancer increases if she is sexually active at an early age, has many sexual partners, or has sex with someone who has HPV or has many partners
- Smoking – Smoking can almost double a woman’s likelihood of developing cervical cancer
- Infection with HIV (Human immunodeficiency virus) – HIV weakens the immune system’s ability to destroy disease-causing agents like HPV, thus increasing the risk of cervical cancer
- Infection with Chlamydia - Studies show that chlamydia may better enable HPV to grow on the cervix, increasing the risk of cervical cancer
- Taking birth control pills - Long-term use of oral contraceptives increases the risk of cervical cancer, though the risk is lowered when use is stopped
- Having multiple children - Women with three or more full-term pregnancies have a higher chance of developing cervical cancer
- Exposure to DES (diethylstilbestrol) - DES was used between 1938 and 1971 as a miscarriage prevention drug. Women whose mothers took this drug while pregnant with them have a higher risk of developing adenocarcinoma of the cervix.
- Family history - A woman’s likelihood of developing cervical cancer increases if she has a family member (such as a mother or sister) who has been diagnosed
HPV and cervical cancer
Various types of high-risk HPV strains are known to cause cancer if not cleared by the body. The HPV-16 and 18 types cause up to 70% of cervical cancers. Tumor suppressor genes in our bodies can control cell growth, but HPV has proteins that can turn off some of these suppressors. This enables cells to replicate abnormally, which can lead to cancer.
While HPV is very common, most women who have contracted it will not develop cervical cancer. Regular screenings will enable your doctor to detect cell changes in the cervix before they develop into cancer, and the HPV vaccine may also help to prevent infection.
Cervical Cancer Prevention
PreventionVarious measures can be taken to reduce the risk of cervical cancers, including:
- Get the HPV vaccine to prevent HPV infection and thus reduce the risk of cervical cancer
- Routine Pap tests can detect cell changes within the cervix. If abnormal changes are observed, doctors can monitor and treat precancerous conditions to help prevent cervical cancer.
- Practice safe sex by using a condom and limiting the number of sexual partners. This will decrease the likelihood of contracting an infection that could cause cervical cancer.
- Using an IUD (Intrauterine device) as a contraceptive has been found to lower the risk of cervical cancer. Consult with a doctor to determine if the benefits of using an IUD outweigh its possible risks.
- Avoid smoking
Medical Marvels: World-Class Care for a Young Mother Facing Cervical Cancer
Eve McDavid, 34, and her husband, Matt, began the year 2020 like many of us: full of hope, unaware that the viral outbreak that was taking hold across the world would change history. They were preparing for a joyous arrival: the impending birth of their second child. At 35 weeks of pregnancy, however, Eve received a surprising diagnosis. She learned she had stage 2B cervical cancer. And it was growing very fast. Thanks to the team of experts at NewYork-Presbyterian/Weill Cornell Medical Center, today Eve is in remission, and their now one-year-old son, Arthur, happily plays with his 3-year-old sister, Ruby Ann, at their home on Long Island.
Trust NewYork-Presbyterian for Cervical Cancer Care
NewYork-Presbyterian is dedicated to cancer care and is home to a team of gynecologic cancer experts ready to assist with your unique needs. We can help identify your cervical cancer symptoms and advise you on the best treatment course if needed.





