August 24, 2016
Over one third of adults in the United States are obese, according to NIH published statistics. The healthcare burden associated with this statistic is drastic, as obesity can lead to various comorbidities and trigger new ones such as type-2 diabetes, fatty liver and cardiac disease. In the quest to treat obesity and improve patient BMI scores, lifestyle modification and pharmacological therapies are frequently unsuccessful. A range of successful bariatric surgical techniques have risen to prominence over the last 30 years, however the number of patients who undergo these surgeries remains limited due to cost, access, and patient concerns.
A new arm in obesity management has risen in the last five years: minimally invasive, endoscopic therapies. Mostly indicated for obese patients who do not fall within the clinical metrics for bariatric surgery, these endoscopic therapies are generally seen as a complement to surgery, not in competition. Endoscopic therapies seek treat patients not eligible for surgery, or do not want to have surgery.
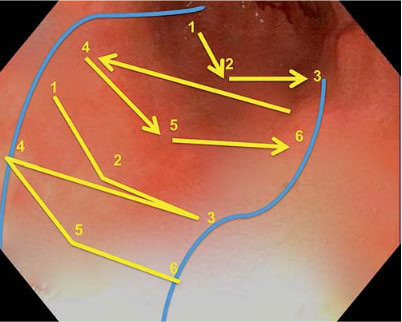
Dr. Reem Sharaiha of the advanced endoscopy team at Weill Cornell was one of the first physicians in the United States to adopt multiple minimally invasive, endoscopic procedures for weight reduction and was one of the first to publish on the use of endoscopic sleeve gastroplasty (ESG). This procedure reduces the volume of the stomach by applying a running pattern of sutures to the interior gastric walls and then tightening them. This effectively constricts the stomach in a tubular fashion, like tightening shoelaces.
Dr. Sharaiha’s first published study on ESG from 2015 included 10 patients. Mean age for the patients was 43.7 years, and the mean excess weight across the population was 70.9 kg. Running sutures were applied in all 10 patients, and the procedure was tolerated well, with no major adverse events occurring. Mild nausea and abdominal pain were observed in 8 patients and chest pain in 2. Mean hospital stay was only 1.3 days, and all patients were able to tolerate an oral diet within 24 hours.
All patients in the study saw weight reduction in the 1-month, 3-month, and 6-monthranges post procedure. Mean excess weight loss across the population was 18%, 26%, and 30% in these respective time periods.
“These initial results pointed to significant improvement in weight loss, and our ongoing work is showing a continued positive effect on BMI, as well as improvement in various comorbidities” said Dr. Sharaiha. “Obesity has secondary influence on so many other things, if we can build a spectrum of therapies, we can treat any level of obesity, reduce comorbidities, and improve overall health and burden on health systems.
Dr. Sharaiha’s research team is set to publish a follow-up study in late 2016. This expands the population of subjects to over 90 and includes clinical protocol refinements as well as metrics at the 24-month mark. Preliminary data demonstrates sustained weight loss over the follow up time period, as well as significant improvement in various comorbidities (systolic blood pressure, diabetes, liver function tests). In addition, Dr. Sharaiha is also testing efficacy of intragastric balloons for weight reduction. Similar to ESG, the intragastric balloon is designed to reduce stomach volume, doing so with silicone balloon placed into the stomach via endoscope, which is then filled with saline. Efficacy research on this procedure is also forthcoming.



