Each year more than 700,000 people around the world die by suicide – one person every 40 seconds – and many more attempt to end their lives. Suicide occurs throughout the lifespan and is the third leading cause of death among 15- to 24-year-olds in the United States and the number one killer of adolescent girls across the globe. Suicide, however, is preventable with timely, evidence-based, and often low-cost interventions. One such measure is the Columbia- Suicide Severity Risk Scale (C-SSRS), a series of simple questions to assess the severity and immediacy of suicide risk that anyone can ask. The scale, also known as the Columbia Protocol, has been translated into more than 150 languages and implemented across all 50 states, across the entire continuum of care (e.g. first responders, schools, justice, healthcare, defense forces, homeless services, and child welfare), national and international agencies and most nations. It is also the common data element for scientific research.

Dr. Kelly Posner
Kelly Posner, PhD, Clinical Professor of Medical Psychology (in Psychiatry) at Columbia, is the lead scientist of the C-SSRS along with researchers at the University of Pennsylvania and University of Pittsburgh. As founder and Director of the Columbia Lighthouse Project, which was formed under the auspices of Columbia to disseminate the C-SSRS, Dr. Posner continues to work with national and international governments and communities on policy and integration of the C-SSRS into their broad suicide prevention programs. “Suicide isn’t a problem of veterans, of kids, or of the elderly. It is our shared crisis of humanity,” says Dr. Posner. “But it is our one preventable cause of death despite the fact that it’s been this tragic paradox that takes more firemen than fire, more police than crime, and more lives than car accidents. Some 135 people are affected by each and every death and those effects linger across generations because of the silence that follows suicide.”
While suicide touches all age groups and ethnicities, there is a continuing global crisis among children, particularly minorities:
- Suicide among 8- to 14-year-olds rose by 150 percent in the last seven years.
- Suicide has increased in African American children in the age range of 5 to 11 years old.
- Between 1999 and 2018, the suicide rate for Black youth ages 10 to 17 rose 87 percent.
- Suicide is the leading cause of death for Asian American/Pacific Islanders ages 15 to 24.
Columbia-Suicide Severity Risk Scale: A Common Method for Risk Detection
While these statistics are alarming, progress is being made to stem the tide of suicide, due in large part to the implementation of the C-SSRS. Supported by the National Institute of Mental Health (NIMH), Dr. Posner and her colleagues developed the screening tool for a 2007 NIMH study of treatments to decrease suicide risk among adolescents with depression. Based on more than 20 years of scientific study, the C-SSRS filled an urgent need to uniformly and reliably identify people who are at risk. Just as important as its ability to identify who might attempt suicide, it was the first tool to assess the full range of a person’s suicidal ideation and behavior, including intensity, frequency, and changes over time.
“The World Health Organization and other global bodies have highlighted for decades that one of the most significant impediments to suicide prevention is lack of a common method of screening,” says Dr. Posner. “One of the greatest impacts of the C-SSRS has been to introduce a common detection method and make it accessible to all across public health. It allows everyone from teachers to parents to clinicians to use a simple set of questions to find those at risk and save lives.”
In 2011, the Centers for Disease Control and Prevention adopted the protocol’s definitions for suicidal behavior and recommended the use of the C-SSRS for data collection. In 2012, the Food and Drug Administration declared the tool the standard for measuring suicidal ideation and behavior in clinical trials. Today, the C-SSRS, which is used in all sectors of the community, public settings, schools, faith communities, hospitals, and the military, is saving lives across the globe on six continents.
Today, the C-SSRS, which is used in all sectors of the community, public settings, schools, faith communities, hospitals, and the military, is saving lives across the globe on six continents.
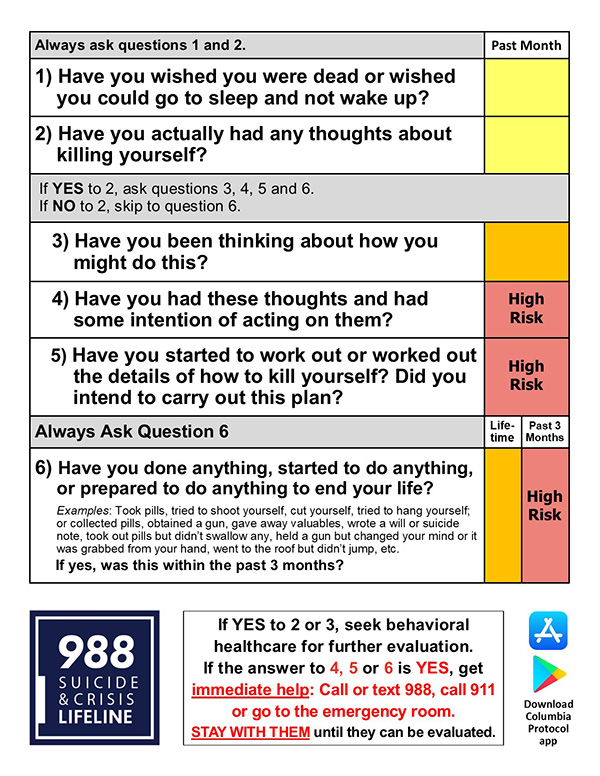
The series of plain-language questions is such that anyone can ask them and the answers help users identify whether someone is at risk for suicide, assess the severity and immediacy of that risk, and gauge the level of support that the person needs. Users of the tool ask an individual:
- Whether and when they have thought about suicide
- What actions they have taken – and when – to prepare for suicide
- Whether and when they attempted suicide or began a suicide attempt that was either interrupted by another person or stopped of their own volition
The number and choice of questions asked depend on each person’s answers. The questioner marks “yes” or “no,” as well as how recently the thought or behavior occurred and scores its severity. The shortest screeners are condensed to a minimum of two and a maximum of six questions, depending on the answers, to most quickly and simply identify whether a person is at risk and needs assistance.
Columbia-Suicide Severity Risk Scale
“There is so much science supporting C-SSRS and one need not be a mental health professional to administer the questions,” says Dr. Posner. “More than 600 peer-reviewed studies have been published supporting the tool’s use in different populations, 50 of which demonstrate predictive validity. In a published study in Psychological Medicine of 18,000 psychiatric emergency patients, scientists in Sweden found that the C-SSRS screener ‘robustly’ predicted death by suicide over one-week, one-month, and one-year periods. Prior to the questionnaire, individuals deemed at risk were routinely sent to hospital emergency rooms on a subjective basis. This approach has its price, as unnecessary referrals can shut down those who need treatment from getting it.”
The simple act of just asking someone in distress how they are feeling can often prevent a tragedy, says Dr. Posner. “We have to empower every citizen to be able to use this method of detection that is vital to saving lives. Everyone can be part of the solution. My friend Kevin Hines, who is now a suicide prevention speaker, survived jumping off the Golden Gate Bridge – which is fatal 99 percent of the time – tells his story. He woke up at age 19 and said to himself, ‘If just one person asks me if I’m okay, I won’t do it.’ Going to the side of the bridge, he was finally approached by someone who asked, ‘Can you take my picture?’ He said, ‘Screw this. Nobody cares.’ and he jumped. Kevin now speaks out on suicide prevention and says, ‘People considering suicide want someone to save them.’
“What we need is a culture where no one is afraid to ask. This is why the C-SSRS is so essential to humanity,” says Dr. Posner. “We have to make it available everywhere. In the past, people didn’t want to ask. They didn’t know what questions to ask. They didn’t know what to do with the answers. They didn’t know if it would be harmful. It’s actually the opposite. When somebody is suffering, they want help. They want to be asked and need to be asked. A life can be saved up until the last minute.”
Transforming the Paradigm in Suicide Risk Assessment
Screening with the C-SSRS in conjunction with other suicide prevention measures is yielding positive results and its use is now policy across all 50 states, national agencies, and most countries. The U.S. Department of Defense cited Dr. Posner’s work as “nothing short of a miracle,” and the Center for Disease Control and Prevention noted that her efforts are “changing the paradigm in suicide risk assessment in the U.S. and worldwide.” Dr. Posner’s scholarly work has been included in the compendium of the most important research in the history of the study of suicide, and in 2018 she was awarded The Secretary of Defense Medal for Exceptional Public Service.
The U.S. Department of Defense cited Dr. Posner's work as "nothing short of a miracle," and the Center for Disease Control and Prevention noted that her efforts are "changing the paradigm in suicide risk assessment in the U.S. and worldwide."
Dr. Posner has been noted in a keynote speech at the White House and has been quoted in Congressional hearings. She also gave the lead presentation in a U.S. Senate forum on school safety after the Parkland tragedy. Through her advocacy, she has helped to change local, national, and international policy, which in turn has helped achieve reductions in suicide across all sectors of society.
“I was so honored that the Columbia Protocol app was recently highlighted by the White House as one of the important ways to help in achieving the President’s mental health initiatives!” says Dr. Posner. “The Columbia Protocol app's ability to help save lives was sent to state legislators as a way to support White House initiatives in identifying those at elevated risk for suicide and directing them to support and care.”
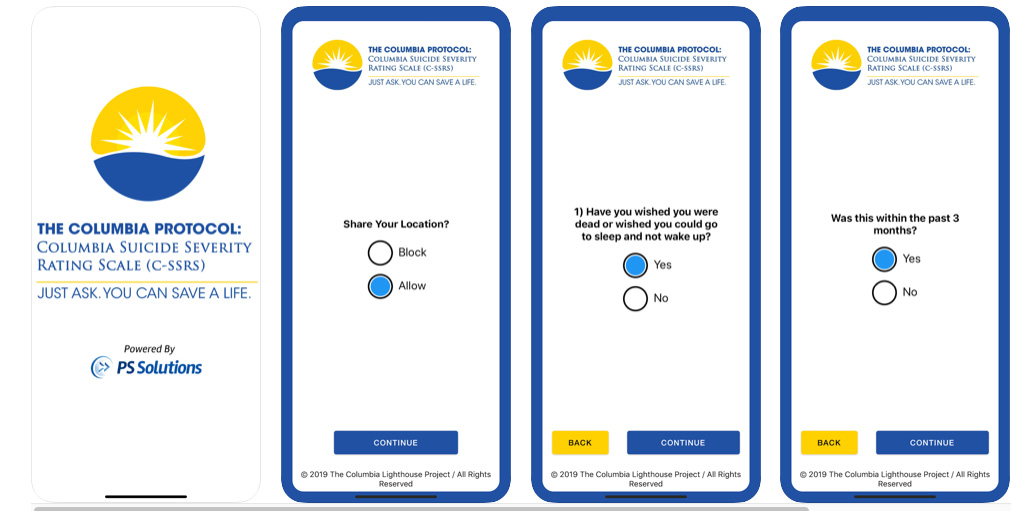
Most recently, the White House announced that the Columbia Protocol app is central to serving its agenda on mental health.
“We know we have to have a public health approach to save lives, and what we know is that 75 percent of people who take their own lives in the United States die at home, and 95 percent of 5- to 11-year-old Black youth who take their lives do it at home,” continues Dr. Posner. “So our policy challenge and what we need to do to really save even more lives is figure out how every home, every parent, and every family member can be equipped with this tool. When I got to give the lead presentation to the Senate after Parkland on school safety, I said, ‘you all have policy for the doctors and the policemen, but how do we get it in all parents', all teachers', and all coaches' hands before they ever – if they ever – get to the doctor.”
“The same way we moved people to wear seatbelts or stop smoking, we need to mobilize at every level to get people to know how to ask simple questions and respond to this public health crisis,” says Keita Franklin, PhD, Co-Director of the Columbia Lighthouse Project and former Director of Suicide Prevention for the Department of Defense and the VA. “The C-SSRS can be administered by anyone, anywhere. It is available as an app downloaded easily and accessed from a mobile phone. What’s become clear is the vital need to have a public health approach to identify people at risk where they work, live, and thrive.”
Quickening Care Delivery Through Linking of Systems Across the Continuum of Care
Dr. Posner and her team point to numerous cases in which the adoption of C-SSRS has impacted suicide prevention methods throughout the United States and within particularly vulnerable populations. Following are just a few examples highlighting the influence of the Columbia Protocol:
- In Tennessee, the statewide adoption of the C-SSRS as the crisis assessment tool, as noted by Melissa Sparks, Director of Crisis Services and Suicide Prevention, Tennessee Department of Mental Health and Substance Abuse Services, “has catapulted a transformation of practices in Tennessee by ensuring professionals and family members who come in contact with an individual who may have thoughts of taking their own life receive the help they need before it is too late.”
- Every policeman has a sticky pad with the Columbia screener and a QR code that connects to Connecticut resources. The Connecticut Alliance to Benefit Law Enforcement worked closely with mobile crisis providers to institute the Columbia Protocol. When communicating with hospitals or mobile crisis upon arrival, the Alliance provides the C-SSRS findings.
Here is one lifesaving example: A school counselor used C-SSRS to identify that a 4th grade boy was suicidal. He was sent to mobile crisis services who confirmed his C-SSRS results, then sent him to a hospital that provided counseling and safety planning. This timely intervention and continuity of care was facilitated by each touch point using the common language of C-SSRS. - What does the new school safety law mean for South Florida students? The district said it is also in compliance with the new law by utilizing the Columbia-Suicide Severity Rating Scale. This tool is the same suicide screening tool used by the local mobile response teams and approved by the Florida Department of Education.
- Firefighters in Texas utilize the C-SSRS in three ways:
- To screen civilians in the community who are potentially suicidal to determine what treatment is appropriate.
- To identify members in the Department who are in need of assistance.
- To recognize family members of firefighters who may be at risk of suicide.
The C-SSRS has become a vital part of health and wellness programs for employees and their families, with a focus on caring for caregivers and front lines workers. In a company of 100,000 employees, every six days, one employee or family member will die by suicide; every day, there are three attempts. Depression is the number one cause of work related absence and costs U.S. workplaces $23 billion annually in lost productivity; 45 to 98 percent of the costs of depression treatment could be offset by gains in work productivity.
We need to treat suicide screening as routine as we do blood pressure. In terms of reducing stigma, we know that asking these questions relieves distress for an at-risk individual.
— Dr. Kelly Posner
“We know that 50 percent of people who die by suicide have seen a primary care clinician in the month before they die,” adds Dr. Posner. “We need to treat suicide screening as routinely as we do blood pressure. In terms of reducing stigma, we know that asking these questions relieves distress for an at-risk individual. Large-scale suicide prevention hinges on the linking of systems and working across all public health sectors.”


