The Gastrointestinal Cancer Prevention and Genetics Program at NewYork-Presbyterian/Columbia is making significant strides towards cancer’s holy grail: the early detection of hard-to-treat cancers. The multidisciplinary program is at the forefront of genetic risk assessment and cancer prevention in familial gastrointestinal syndromes that raise the risk for pancreas, gastric, and colon cancers.

Dr. Fay Kastrinos
Led by Fay Kastrinos, MD, MPH, a gastroenterologist at NewYork-Presbyterian/
Targeting a growing threat

Dr. Sheila Rustgi
Pancreatic cancer, which kills almost 50,000 people each year, is a major focus. Rates of the disease are on the rise and it is predicted to be the second most common cause of cancer death, behind lung cancer, by 2030.
“Pancreatic cancer is really tough because it's very difficult to detect,” says Sheila D. Rustgi, MD, a gastroenterologist at NewYork-Presbyterian/
A number of hereditary cancer syndromes can increase the risk of malignancy, including but not limited to, hereditary breast and ovarian cancer syndrome (BRCA 1 and BRCA 2 gene mutations), Lynch syndrome, and familial atypical multiple mole melanoma. “About 10% of pancreatic cancer patients have some kind of familial component,” says Dr. Rustgi. “That includes patients who have a strong family history of pancreatic cancer and patients who have an underlying genetic mutation.”
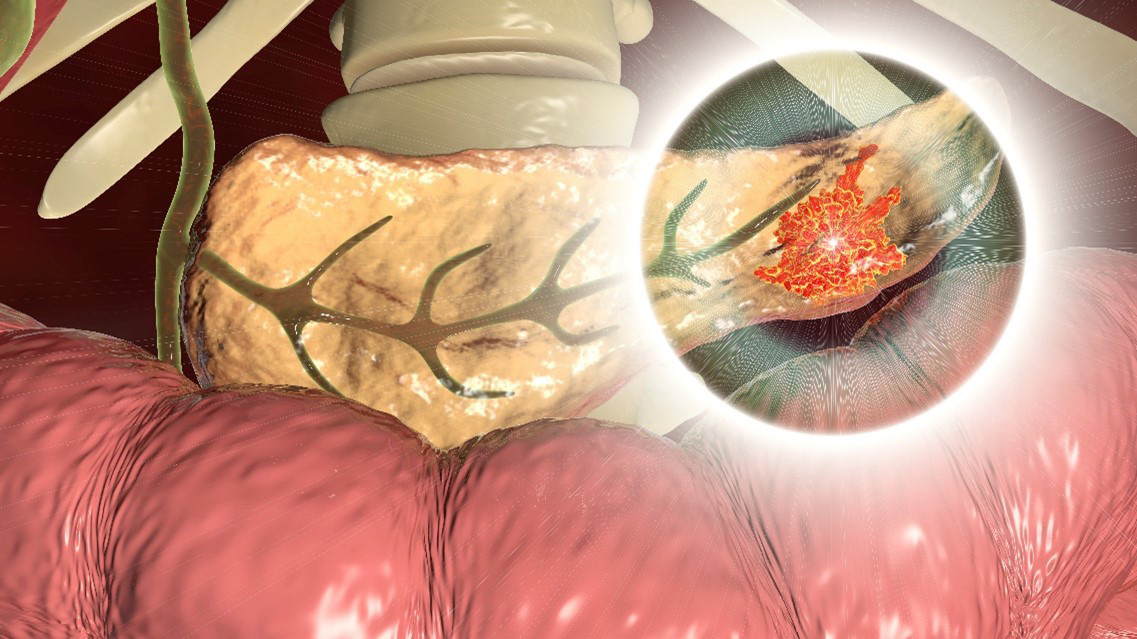
Malignant tumor in the pancreas
According to new guidelines, anyone diagnosed with pancreatic cancer should receive germline genetic testing to identify any inherited gene alterations. The tests can be used to alert other family members to a possible increased cancer risk as well as to steer treatment. “These guidelines were driven by the more favorable response to certain treatments in pancreatic cancers that are due to these genetic predispositions,” says Dr. Kastrinos.
About 10% of pancreatic cancer patients have some kind of familial component. That includes patients who have a family history of pancreatic cancer and patients who have an underlying genetic mutation.
— Dr. Sheila Rustgi
High-risk patients in the program each year receive either magnetic resonance cholangiopancreatography (MRCP), a special type of MRI that visualizes the biliary and pancreatic ducts, or an endoscopic ultrasound, which transmits ultrasound waves internally to view the pancreas, says Dr. Kastrinos.
The benefits of surveillance
As part of the Cancer of Pancreas Screening-5 (CAPS5) consortia, NewYork-Presbyterian/
Over the course of the study, there were 10 diagnosed cases of pancreatic cancer. Among patients in the program, seven had stage I tumors. One was diagnosed at stage II and another at stage III. The remaining cancer patient left the surveillance program and was diagnosed with advanced cancer four years later. “Surveillance programs work,” says Dr. Rustgi.
NewYork-Presbyterian/
“We participate in both because we feel that that the more we know from our high-risk individuals about screening, the better we can inform guidelines, the better we can also test screening strategies and validate new biomarkers,” says Dr. Kastrinos. “Also, we have families that have striking histories without identified gene mutations. So it opens the door to new gene discovery. It all comes from the hard work of multiple institutions working together in these consortia.”
We participate in [research consortia] because we feel that that the more we know from our high-risk individuals about screening, the better we can inform guidelines, the better we can also test strategies and validate new biomarkers.
— Dr. Fay Kastrinos
Dr. Kastrinos’ team uses simulation modeling to advance knowledge as well. “Prospective longitudinal studies take many years and many patients to complete,” she says. “We are focusing on simulation modeling to inform guidelines and clinical management, and determine cost effectiveness.”
The power of prevention
Intensive screening and surveillance is also critical for people with gastric and colon cancer. Hereditary diffuse gastric cancer, which also confers a greater risk for breast cancer, is caused by an alteration in the CDH-1 gene. The cancer usually affects the entire stomach rather than one part of it.
“The risk for gastric cancer is high among carriers with pathogenic variants in the CDH-1 gene and it spans across multiple generations,” says Dr. Kastrinos. “We do intensive screening with endoscopy and also recommend risk-reducing surgeries like prophylactic gastrectomy as a method to keep select high-risk individuals cancer free.”
Although rates of colon cancer are dropping overall, early-onset cancers—those that develop before age 50—are on the rise. As a result, “the United States Preventive Services Task Force recently recommended to start screening people at the age of 45 instead of 50,” says Dr. Rustgi.
Illustration of colorectal cancer
Early-onset colon cancers can frequently have a genetic origin, says Dr. Kastrinos. “In people over 50 diagnosed with colon cancer, about 3-5% of individuals will have an inherited gene alteration, predominantly for Lynch syndrome,” she says. “In individuals younger than age 50 , about 10% will have Lynch syndrome, and in those less than 35 years old, that number goes up to nearly 25% for Lynch syndrome.”
Colonoscopy has the benefit of not only detecting cancer but preventing it by removing precancerous lesions and polyps, Dr. Kastrinos says. However, removal of the colon may be necessary to manage some high-risk conditions, including familial adenomatous polyposis, which causes multiple adenomatous polyps and can lead to colon cancer and malignancies in other digestive organs.
“Our surveillance programs are focused on balancing the benefits and risks of screening and other risk-reducing interventions such as surgery,” says Dr. Kastrinos. “The goal is to detect cancers at an early stage so patients have the most favorable outcomes.”




