
Juan P. Rocca, MD, MHA
NewYork-Presbyterian/
“For cases with disease limited to the liver only, we know that if we can eradicate that disease in the liver, patients can have the benefit of not having to depend on systemic treatments, like chemotherapy or immunotherapy, to control the disease,” says Dr. Rocca. “This can prolong significantly their survival and improve their quality of life.”
The third most diagnosed cancer in the United States, colon cancer is the second most common cause of cancer deaths globally. Data show that up to 25% of patients are diagnosed with stage IV disease, and liver metastasis is present 15-25% of the time. In 70-80% of these cases, metastasis is confined to the liver.
For cases with disease limited to the liver only, we know that if we can eradicate that disease in the liver, patients can have the benefit of not having to depend on systemic treatments, like chemotherapy or immunotherapy, to control the disease. This can prolong significantly their survival and improve their quality of life.
— Dr. Juan Rocca
In those with colorectal cancer liver metastases (CRLM), liver transplantation could offer hope when it isn’t possible to remove cancer from the liver by surgery or other interventions, leading to a poor prognosis. “Sometimes we cannot remove all the disease, because there are too many tumors spread throughout the liver or the tumors are too close to certain delicate structures of the liver and critical blood vessels,” Dr. Rocca says.
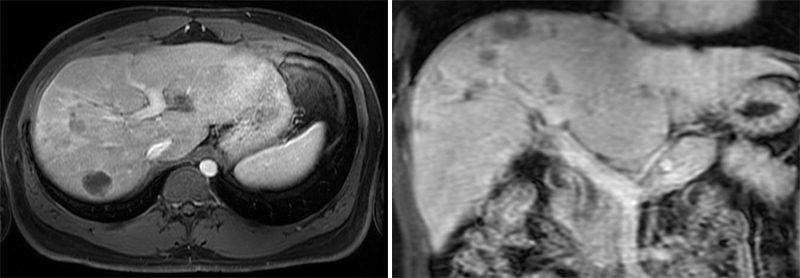
MRI of colorectal cancer liver metastases.
And even when surgery is feasible for multiple tumors, there is a high risk of the cancer recurring. “There are some biologic factors in the microenvironment of the liver that allow those tumors to keep growing there,” says Dr. Rocca. “By removing the liver, we are removing the microenvironment that is allowing cancer to grow into that liver, and you may have a better control of the disease in the future.”
A Long History of Liver Transplantation
The innovative treatment approach builds on decades of experience of transplantation for other liver-related conditions and cancers. “In the 90s, we learned that if you transplanted someone for a primary liver cancer within a certain size, the survival rate was as good as if the patient had no cancer,” says Dr. Rocca. “In the 2000s, we added other diseases and established more criteria. We are slowly expanding our transplantation criteria to different cancers.”
Interest in liver transplantation for metastatic colon cancer is a more recent focus. Norwegian research has shown a 60% to 83% five-year survival rate in patients undergoing liver transplants for CRLM, the latter figure reflecting more restrictive selection criteria. Strict eligibility requirements are particularly important in the U.S., where donor livers are a scarce resource. “Our organ allocation system cannot yet give colorectal cancer a priority in terms of proven survival benefit like for other traditional indications,” says Dr. Rocca. “While the US system allows colorectal cancer patients to receive a liver transplant, they are at the bottom of the waitlist.”
Adding metastatic colon cancer to the list of indications for liver transplants has been accelerated by progress on several medical fronts. These include the introduction of immunotherapy, better oncologic protocols, and advances living donor liver transplantation as well as in the preservation of donor livers, specifically machine perfusion pumps, which allow surgeons to use livers that were previously considered unsuitable for transplantation, Dr. Rocca says.
“The [perfusion] pump circulates blood and lets the liver work again before transplanting it, and we can measure all the things that we consider very important for proper liver function, like how it clears lactate, the production of bile, and other parameters,” says Dr. Rocca. “We keep the liver on the pump from six to 24 hours and then can proceed with the transplant and know that the liver is going to work. We are expanding the donor pool this way.”
Integrating innovations in surgery has also made a difference. The team developed robotic surgery protocols for liver cancer surgery, living donor liver surgery and liver transplantation, expanding the benefit of a minimally invasive approach to all patients. “We're getting better results, because we're able to align so many different technologies into treating our patients better,” Dr. Rocca says.
Full Spectrum, Multidisciplinary Care
Colon cancer patients with liver metastases may access a variety of treatments. “Our team can offer patients everything from the least invasive treatment to a liver transplant,” says Dr. Rocca. “One of the keys for success in the field of transplant oncology is to be able to offer the entire spectrum of treatments and see what combination will be best for long-term survival for each specific case.”
Transplantation is limited to those most likely to benefit and to make the most of scarce organs. “We’re very careful in how we select our patients. We’ve considered more than 30 patients but only five made it to transplant,” Dr. Rocca says. “The estimate is that only about 2% of patients with metastasis to the liver from colorectal cancer end up with an organ transplant.” Nonetheless, many of the patients that couldn’t make it to transplant still benefited from a dedicated multidisciplinary care that prolonged their survival.
To be considered, patients must have received the cancer diagnosis more than a year’s time and surgery to remove the primary tumor performed at least six months before. Imaging tests of the chest and abdomen are needed to confirm that the disease has metastasized only to the liver. Patients receive chemotherapy, immunotherapy, and locoregional therapies like radiofrequency ablation and radio-embolization, which work synergistically with immunotherapy to reduce liver tumors up to the time of transplant evaluation.
With colorectal cancer, there is a lot of shedding of DNA in the bloodstream, which is something that we're able to capture using liquid biopsy. It allows us to genomically identify the type of colon cancer patients have, the mutations that make up the colon cancer, in order to monitor the progress of treatment.
— Dr. Pashtoon Kasi
“We need to keep the tumor at bay while we complete the workup for transfer to the transplant list,” says Dr. Rocca. “At the same time, there is a psychosocial evaluation to make sure that patients can take care of the new liver after transplantation.” After a patient is placed on the wait list, new imaging tests are needed every three months to catch any new malignancy.
New Tools to Monitor for Recurrence
A new indispensable tool also integrated in the process is a test called liquid biopsy, which, unlike a tissue biopsy, uses a noninvasive blood draw to collect tumor DNA circulating in a patient’s blood. This technology, known also as circulating tumor DNA (ctDNA) testing, allows doctors to determine the genetic makeup of cancers quickly and easily, and track progress over time.

Pashtoon Kasi, MD
“With colorectal cancer, there is a lot of shedding of DNA in the bloodstream, which is something that we're able to capture using liquid biopsy,” says Pashtoon Kasi, MD, an oncologist and the Director for Liquid Biopsy Research at the Englander Institute for Precision Medicine at NewYork-Presbyterian/
One of the utilities of liquid biopsies are useful in determining whether all cancer has been eliminated from a patient’s body after any procedure seeking elimination of cancer. “It’s possible that there’s a small cancer below the resolution of the imaging studies we use to decide to do surgery or transplant” Dr. Rocca explains.
Dr. Kasi adds, “Key to success is selecting the right patients who would benefit the most from this approach. It is important to give the test of time in terms of making sure that the cancer is well controlled. Furthermore, integrating these liquid biopsies can potentially help in assessment of disease burden and ongoing response to therapy. The traditional tumor markers, like CEA or CA-19-9, are not always reliable. Furthermore, these liquid biopsy assays can also be used in the surveillance setting post-transplant. We are one of the few centers utilizing this as another tool in our toolbox for these patients.”
Such multi-disciplinary collaborations and constant evaluations are extraordinarily important. At NewYork-Presbyterian/
“We are careful when we expand the criteria for treating liver cancer, because cancer comes back,” Dr. Rocca says. “And then we start thinking this precious gift of life should probably go to someone else. That's why the way we advance transplantation for liver cancer is slowly and cautiously.”
Dr. Kasi adds, “In some situations, having had a transplant can potentially take away future clinical trials and other options. So, the decision is not straightforward and is a process of ultra-hyper-selection to identify the patients who would benefit the most from such an approach.”





