The incidence of fetal cardiac tumors is less than 1%, but physicians at NewYork-Presbyterian/Columbia see these tumors as often as once a month. However, even they were surprised when a pregnant woman at 33 weeks’ gestation presented with an unusually large fetal cardiac mass that measured 3.3-by-3.2-by-2.5 cm.
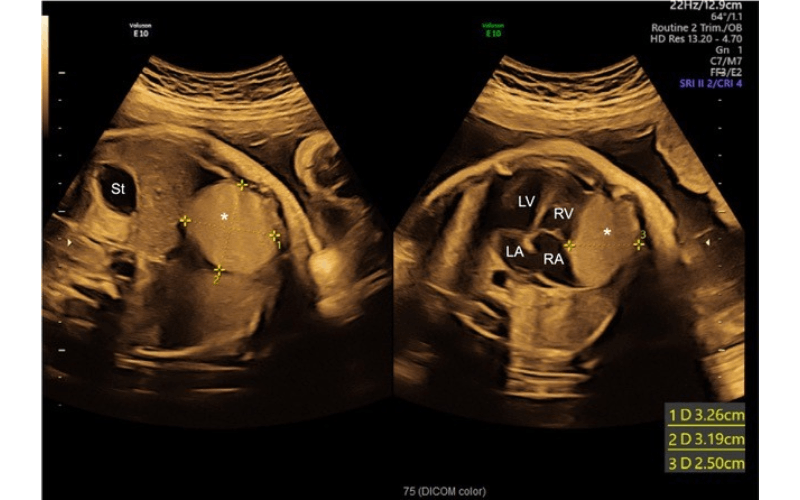
Transabdominal ultrasound demonstrating a giant cardiac tumor measuring 3.3-by 3.2-by-2.5 cm.
Below, members of the patient’s NewYork-Presbyterian/Columbia care team – pediatric cardiologist Julie Glickstein, MD, maternal-fetal medicine specialist Maria Andrikopoulou, MD, PhD, and maternal-fetal medicine fellow Nicole Krenitsky, MD, MBA – share details of the case and how it reinforces the benefits of having a multidisciplinary team in place.
How the Patient Presented
This patient was referred to us from an outside institution who came in with a completely different diagnosis of a suspected fetal lung mass. We met her at 33 weeks’ gestation. We performed an ultrasound scan, and we had a suspicion that this was a cardiac tumor, not a fetal lung mass. She was seen by both maternal-fetal medicine and cardiology on the same day, and the pediatric cardiology team confirmed that this was a cardiac tumor and provided more information about the fetal heart function, which was normal thus far. Following the diagnosis, the mother was followed very closely through the rest of her pregnancy until her scheduled induction at 38 weeks.
Risks
In this patient, fetal growth was normal; however, the concern was that cardiac tumors, when they are very big like this one was, can impact cardiac function, cause cardiac failure, or obstruct the outflow tracks. They can also cause heart failure that presents in the fetus as hydrops. The mother was followed very closely with weekly ultrasounds and echocardiograms to make sure that the baby did not have any decompensation and heart failure.
Making the Diagnosis
When evaluating cardiac tumors both pre and postnatally there is a differential diagnosis of different types of tumors. We suspected based on the prenatal MRI and fetal echocardiographic images that this was a cardiac rhabdomyoma. However, this case was unique and challenging because rhabdomyomas are usually in the heart cavities. These specific tumors can be single or multiple. This rhabdomyoma, however, was in the pericardial sac. Getting the prenatal diagnosis right is important because usually rhabdomyomas regress after birth and they can just be observed, whereas other fetal tumors require surgery. Rhabdomyomas can also be associated with a genetic diagnosis of tuberous sclerosis. We performed a cardiac MRI postnatally at two days of age, which was more definitive based on tissue characterization, and confirmed the rhabdomyoma diagnosis.
Fetal echocardiogram of four chamber view demonstrating a large homogeneous mediastinal mass adjacent to the right ventricle and right atrium in the pericardium with partial compression of the right ventricle.
Patient Prognosis
The mother’s labor and birth were unremarkable. The baby was born healthy and was followed with echocardiogram and frequent outpatient cardiology visits to make sure she was growing, gaining weight, and meeting her developmental milestones. Her case was discussed with our entire cardiology group and the cardiothoracic surgeons and, as of now, there is no indication for removal of the tumor. The mass is not currently affecting her cardiac function or her growth and development. She has had no arrhythmias or abnormal heart rhythms. We are optimistic that she will continue doing well. The mass has gotten slightly smaller over her first year of life. As she gets older, we will repeat her cardiac MRI and we expect this rhabdomyoma will only get smaller.
Lessons Learned
This case challenged our clinical decision-making and diagnostic abilities because it was so unique. It was a great reminder to think outside of the box and recognize things that may not be presenting like you read in the textbook. But mostly, it underscored how privileged we are to work at a center like NewYork-Presbyterian/Columbia, where we place the patient at the center of the spoke model.
When this patient came in, she was able to receive multidisciplinary care right away. The same day, all three of us were able to sit down, scan the patient, talk about her case and come to a consensus. In the week after that, the patient met with the pediatric cardiothoracic surgery team. We also referred her to genetics, in case there was a genetic component, and then she was also able to meet with our neonatology team to talk about what the impact would be after the baby was born. All the teams came together to support her and her future baby while collaborating closely with each other to ensure we achieved the best outcome.