Diabetes mellitus is an independent predictor of whether patients will develop spinal cord injury following open descending thoracic aneurysm (DTA) and thoracoabdominal aneurysm (TAAA) repair, according to a recent study conducted by physicians at NewYork-Presbyterian/Weill Cornell Medicine.
Permanent spinal cord injury, typically resulting in either paraparesis or paraplegia, is a well-known and devastating complication of DTA/TAAA surgery and is estimated to occur in nearly 6% of cases across the nation.
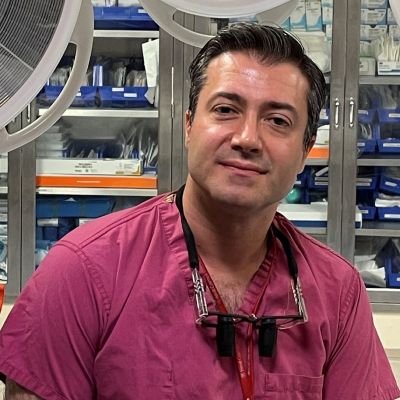
“If you ask these patients what they fear the most when they are advised to undergo surgery, most of them will say that they fear remaining in a wheelchair for the rest of their lives even more than dying,” says Ivancarmine Gambardella, MD, lead author of the study and a cardiothoracic surgeon at NewYork-Presbyterian/Weill Cornell Medicine. “I have the tremendous opportunity of conducting research on one of the biggest cohorts of DTA/TAAA replacements. Thanks to the vision and relentless dedication of Dr. Girardi, chairman of our department and my mentor, I can investigate on a series of DTA/TAAA surgery patients that presents the lowest rates of spinal cord injury and mortality worldwide.”
Making DTA/TAAA Surgery Safer
Over the last few decades, surgeons have tried various ways to decrease the rate of spinal cord injury, from modifications to surgical technique to drainage of cerebrospinal fluid. Dr. Gambardella says NewYork-Presbyterian/Weill Cornell Medicine already has one of the lowest rates of spinal cord injury in the country, but he and his cardiothoracic surgery colleagues are aiming to drive it even lower.
The recent study aimed to improve the safety of DTA/TAAA surgery by investigating how diabetes is linked to the risk of spinal cord injury. In past research on spinal cord injury in DTA/TAAA repair at NewYork-Presbyterian/Weill Cornell Medicine, diabetes has repeatedly come up as an associated factor. “That made me think of digging deeper into this to see if it was an independent risk factor for spinal cord injury,” says Dr. Gambardella.

Normal versus aneurysmal thoracoabdominal aorta.
Dr. Gambardella and his colleagues compared the preoperative variables and postoperative outcomes for 934 patients with and without diabetes who underwent open DTA/TAAA repair from July 1997 to April 2021 at Weill Cornell Medicine’s Department of Cardiothoracic Surgery. The researchers individually propensity-score matched 92 patients with diabetes with 184 non-diabetic patients so that preoperative and intraoperative variables were similar between the two groups.
Overall, 6.5% of patients with diabetes experienced spinal cord injury, compared with just 1.6% of patients without diabetes. Diabetes was also associated with a higher rate of operative mortality at 14.1%, versus 6.0%.
Using conditional logistic regression, Dr. Gambardella and his colleagues confirmed that diabetes independently increases five-fold the risk of spinal cord injury (odds ratio 5.5).The findings were published in the Annals of Surgery. “This is very important because we can do something about this finding,” says Dr. Gambardella.
What we know is that when we do these operations we need to make a big effort to ensure that the blood glucose of these patients is kept in check because what is at stake is the usage of their legs. This is something that we can already put into practice.
— Dr. Ivancarmine Gambardella
The first line of defense is to keep patients under strict glycemic control in the perioperative period, regardless of diabetes diagnosis.
“What we know is that when we do these operations we need to make a big effort to ensure that the blood glucose of these patients is kept in check because what is at stake is the usage of their legs,” says Dr. Gambardella. “This is something that we can already put into practice.”
Stress-induced perioperative hyperglycemia can be managed through deep analgesia as part of anesthesia in surgery and immediately in the postoperative period. Medication-induced hyperglycemia can be counteracted by reducing corticosteroids and adrenergic agonists and increasing intravenous fluid administration and non-catecholamine vasopressors, according to Dr. Gambardella.
The next way that physicians can apply the findings on diabetes and spinal cord injury is to provide an alternative energy source to glucose, protecting patients from hyperglycemia while also ensuring they are well nourished in the peri-operative period.
Dr. Gambardella and his colleagues recently performed a meta-analysis that showed that ketosis had a potent neuroprotective effect during acute injury of the central nervous system in animal studies published in the Journal of Neurochemistry. In these patients, such protective effect could not be reasonably achieved through a ketogenic diet (for lack of compliance) or intermittent fasting (for its catabolic effects). However, exogenous ketones offer potential as a glucose alternative.
Peroxisome proliferator activated receptor (PPAR) agonists are a class of medications that have also been shown in animal models to reduce spinal cord injury. Dr. Gambardella says this is another promising avenue of investigation and is in the process of finalizing a meta-analysis of PPAR agonists as neuroprotective agents.
“We want to meta-analyze this evidence, and if we see that PPAR agonists are beneficial, we are thinking of doing an experimental study in animals, where we give both the ketones and PPAR agonist and see if this gives an even bigger benefit, compared to only ketones or only PPAR agonists. If this proves to be the case, we could proceed with a randomized controlled trial in humans,” says Dr. Gambardella. “Finally, we are also thinking of investigating whether an extra-peritoneal surgical approach can significantly reduce the loss of peritoneal fluid and therefore the need for adrenergic vasopressors that cause hyperglycemia.”