Pelvic floor pain and dysfunction are often linked to a range of disorders and conditions, making these conditions challenging to diagnose. Little cross-collaboration among specialty providers leaves patients often consulting with varying specialists in seeking relief. “Many of my patients will have seen multiple specialists, including urologists, gynecologists, urogynecologists, and gastroenterologists before coming to me,” says Jaclyn H. Bonder, MD, a physiatrist and Medical Director of Women’s Health Rehabilitation at NewYork-Presbyterian/
Dr. Jaclyn Bonder
“I entered the field as a women’s health rehabilitation specialist and over time my practice evolved to include patients with musculoskeletal conditions, such as back, hip, and joint pain related to pregnancy and being postpartum, and pelvic pain and pelvic floor dysfunction at any point in a woman’s life span,” she says. “I also see patients with abdominopelvic pain that extends anywhere from the umbilicus to the gluteal fold in the pelvic girdle area.”
Dr. Bonder is among a handful of physicians nationwide who specialize in women’s health rehabilitation with a pelvic floor and antepartum focus. She treats numerous pregnant and postpartum patients with musculoskeletal problems, as well as those with other conditions related to pelvic floor muscle dysfunction and weakness. These include chronic pelvic pain, urinary and bowel issues, pain following gynecologic surgery, dyspareunia, and pain in the lower back, groin, abdomen, and hips. “Patients can present with pelvic pain, pelvic girdle pain, or pelvic floor pain. It is important to realize that there is a large musculoskeletal component to pelvic girdle and pelvic floor pain.”
According to Dr. Bonder, physiatrists are uniquely qualified to manage these patients because of their knowledge of the musculoskeletal and nervous systems and awareness of the relationships among pain, physiology, and function. “Pelvic pain can have multiple etiologies but in all of them the muscles, joints, and nerves of the pelvis are almost always affected, either primarily or secondarily,” says Dr. Bonder.
“Pelvic pain can have multiple etiologies but in all of them the muscles, joints, and nerves of the pelvis are almost always affected, either primarily or secondarily.” — Dr. Jaclyn Bonder
Dr. Bonder’s practice spans a wide range of patients from 18 to 85 – from young women becoming sexually active and experiencing dyspareunia and vulvodynia, to women of childbearing age with nerve pain following a vaginal delivery, to middle-aged women and those who are post-menopausal who often have pelvic and vaginal pain due to loss of estrogen or architecture changes related to menopause.
“Diagnostically, I’m trying to determine if the pain and/or dysfunction is originating with a joint, nerve, or muscle of the pelvis,” says Dr. Bonder. “The examination may include X-rays or an MRI of the pelvis, hip, or lumbosacral plexus, which is usually where we look more at the nerves of the pelvis.”
With chronic neuropathic pain syndromes, Dr. Bonder evaluates the nerve roots and the muscles the nerves innervate. “For example, with pudendal neuralgia, there are several possible sites of primary traction, compression, and entrapment. Etiologies can range from iatrogenic injury during pelvic surgery to cycling and compression from prolonged sitting,” she says. “It also may be associated with bladder, bowel, or sexual dysfunction.”
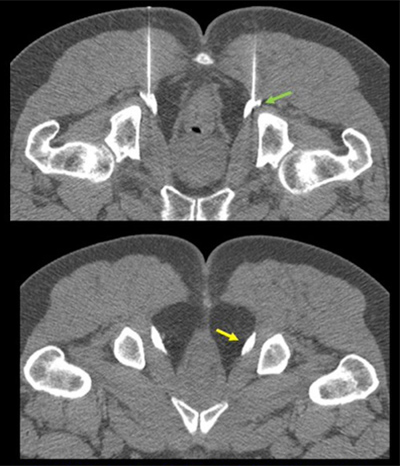
CT guided, bilateral pudendal nerve blocks using 22-g needles and administration of kenalog and bupivacaine. Yellow arrow indicates distension of Alcock canal with medications.
To address the multiple causes of pelvic pain, Dr. Bonder calls on a range of non-surgical treatment modalities that include:
- Pelvic floor physical therapy
- Central nervous system medications
- Topical agents
- Valium suppository
- Botulinum toxin injections
- Trigger point injections
- Selective peripheral nerve blocks
Dr. Bonder points out that frequently pelvic pain is not necessarily related to the organs of the pelvis. “It’s very possible it is muscular, neurologic, or neuropathic in nature,” she says. “Even patients with bladder pain and spasms who feel they have a UTI many times can be pelvic floor muscle related. It’s not what patients or doctors often think of as a cause or source of the pain. My hope is that clinicians will recognize the role physiatrists can play in diagnosing and treating these conditions and refer accordingly.”



