Fatigue is a common symptom of interstitial lung disease (ILD) but there is limited knowledge about how to evaluate it, leading to both underdiagnosis and undertreatment. However, new research from NewYork-Presbyterian/

Kerri Aronson, MD, MS
“Fatigue is multifactorial and it’s something we don’t have a great understanding of in terms of what may be causing it, how to evaluate it, or how to treat it. That’s pretty common in other chronic diseases and it’s certainly true in interstitial lung disease,” says Kerri Aronson, MD, MS, assistant professor of medicine in the division of pulmonary and critical care medicine at NewYork-Presbyterian/
One reason that fatigue has not been incorporated into ILD research studies is that there has not been a valid way of measuring it. As a result, clinicians and researchers often use objective clinical measures, such as lung function tests, which can create an incomplete picture, Dr. Aronson says. A patient with ILD could perform well on a lung function test but still feel fatigued.
Additionally, just asking if a patient is experiencing fatigue is unlikely to be specific enough. “In chronic lung disease, patients sometimes think that breathlessness is the same as fatigue, but what we’re talking about here is lack of energy,” Dr. Aronson says. Having a specific patient-reported measure of the type of fatigue – such as mental or physical exhaustion – and the degree of it, is the best way to accurately measure this outcome, she said.
The Fatigue Severity Scale (FSS) is a nine-item, patient-reported questionnaire that assesses how the patient perceives their fatigue severity and how it impacts physical functioning and family, work, and social activities. The questionnaire was designed to measure fatigue in patients with chronic neurologic disease but has since been validated in several other chronic illnesses. Dr. Aronson, who is an expert in patient-centered outcomes research in ILD and has developed other patient questionnaires, sought to evaluate use of the FSS among patients with ILD.
Dr. Aronson and her colleagues used data from more than 1,800 patients with ILD in the Pulmonary Fibrosis Foundation Patient Registry to measure the reliability and validity of the FSS compared with other validated patient scales measuring quality of life and shortness of breath, as well as clinical measures such as pulmonary function and six-minute walk distance. The FSS was shown to be correlated with other measures related to fatigue and was able to distinguish between patients with different fatigue severity. The findings were published in the American Journal of Respiratory and Critical Care Medicine.
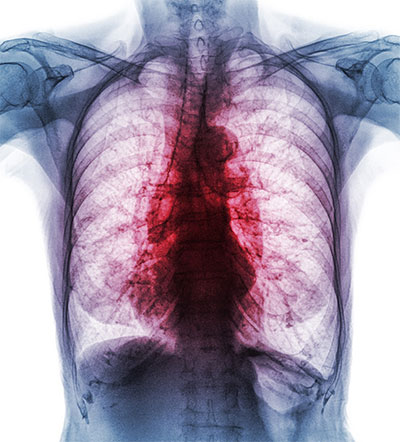
Interstitial lung disease causes inflammation or scarring of the lung tissue.
The analysis showed that FSS had a moderate to strong correlation with energy levels and shortness of breath, but a weak correlation with physiological measures such as forced vital capacity, diffusing capacity of the lung for carbon monoxide, and a six-minute walk distance. While not a surprise to the researchers, this was an important finding, Dr. Aronson says.
The Fatigue Severity Scale (FSS) is a nine-item, patient-reported questionnaire that assesses how the patient perceives their fatigue severity and how it impacts physical functioning and family, work, and social activities.
“We believe that adds to the argument that lung function is important to measure but it doesn’t capture a lot of the nuances of the impact of the disease. We need these other measures to be able to capture that,” she says.
Importantly, lung function is the most common endpoint in clinical trials of ILD. Along with validating the FSS, this new research highlights that lung function is likely not the best way to capture an outcome important to patients – fatigue. “If we only go by lung function, we’re going to be missing what matters,” Dr. Aronson says.
The FSS has cleared the first hurdle toward its use in ILD clinical practice and research, but more testing needs to be conducted. The registry analysis was able to show the effectiveness of the FSS in establishing the baseline level of fatigue and its severity, but additional studies are needed to understand its responsiveness over time. The next step would be to evaluate the FSS in the controlled setting of a clinical trial to gather more information on what constitutes a clinically meaningful change in the fatigue score, Dr. Aronson says.
“If we only go by lung function, we’re going to be missing what matters.” — Dr. Kerri Aronson
Along with establishing the validity of the FSS, the study raised some other important questions about the treatment of ILD, Dr. Aronson said. For instance, the analysis examined FSS scores by medication and found that patients taking steroids had much higher fatigue scores than patients who were not on steroids. While steroids are not typically used to treat ILD, another future research question could be how medications in ILD may be contributing to symptoms of fatigue, Dr. Aronson says.
“Even with some of our other medicines that we use specifically to treat ILD, fatigue can potentially be one of the side effects, so it’s worth thinking about whether medications are causing fatigue or making it worse,” she says.




