With a strong presence in neurology, orthopedic surgery, and rehabilitative medicine, the Weinberg Family Cerebral Palsy (CP) Center at NewYork-Presbyterian/
“Cerebral palsy is an injury to the developing brain. Spasticity and the increased tone that comes with the injury leads to secondary deformations of the joints,” says Jason B. Carmel, MD, PhD, Executive Director of the Weinberg Family CP Center. “In many cases, the earlier we intervene, the better the outcomes. Our strength is seeing patients across all three disciplines to give the best treatment options.”
Translational Medicine
As a pediatric neurologist and motor system neuroscientist, it is not lost on Dr. Carmel that CP Centers are usually directed by orthopedic surgeons. “Because I am a neurologist, I am interested in nervous system repair and that makes our approach unusual. Our center is unique in having a basic science center attached to a [CP] center,” says Dr. Carmel.
The integration of clinical care and science is ever present at the Center. Dr. Carmel’s Lab, called the Movement Recovery Laboratory, focuses on translational studies where stimulation- and activity-based repair strategies are modeled in young animals with early brain injury. The group then translates findings to humans, with the ultimate goal of designing better treatments for people with CP and other debilitating conditions.
Novel Therapies
The Lab’s unique approach focuses on promoting movement recovery in CP by using brain and spinal cord stimulation. Although noninvasive spinal cord stimulation has previously been used for pain, researchers like Dr. Carmel are now applying it to restore movement. Typically, neuromodulation procedures, including selective dorsal rhizotomy or intrathecal baclofen pump, have been used for the treatment of spasticity associated with CP. By strengthening nervous system connections, stimulation represents a departure from the standard of care because it is working to repair the nervous system.
In his most recent paper appearing in the Journal of Neurophysiology, Dr. Carmel and colleagues used electrical stimulation to elicit and map arm and hand muscle responses in humans. This map can then be used to guide electrical stimulation as therapy. The researchers are now applying the paired brain and spinal cord stimulation that was effective in rats to people. The study seeks to fill critical gaps in our understanding of the plasticity of the sensorimotor system and strategies to strengthen connections after injury. This study was sponsored by grants from the National Institutes of Health and the Travis Roy Foundation.
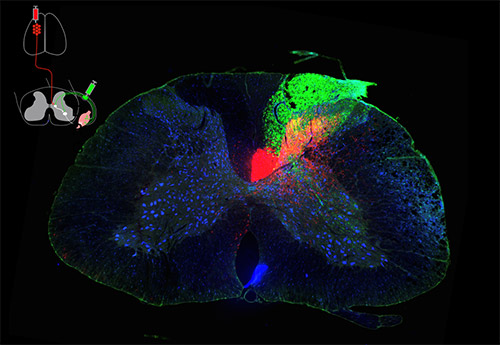
Descending motor (red) and segmental afferent (green) axons terminate onto cervical spinal cords neurons (blue) cord in the rat. These connections were coactivated to produce spinal cord associative plasticity.
(Source: Image courtesy of HongGeun Park, PhD, working in the lab of Jason Carmel, MD, PhD.)
“In humans, we have tested this protocol in individuals undergoing spinal surgery. Our mechanistic study is helping us to better understand how pairing brain and spinal cord stimulation can be combined,” says Dr. Carmel, who has performed the procedure in about 80 adult patients to date. “We are planning the translation to children using non-invasive techniques,” he adds.
By stimulating spared motor circuits, the researchers are able to better understand and map muscle responses to spinal circuits, as well as target interventions to activate movement and strengthen damaged spinal circuits. “Our approach differs from previous approaches in the field because we are using stimulation of brain and spinal cord to make it stronger,” says Dr. Carmel, who notes that the majority of spinal stimulation has previously been performed in adults with spinal cord injury, multiple sclerosis, and Parkinson’s disease.
“Basic science explorations like these allow us to stay up to date with all of the possibilities for best-in-class care of patients with CP who present for orthopedic care at New York Presbyterian,” says Director of Pediatric Orthopedics at NewYork-Presbyterian/Columbia and Chief Quality Officer, Columbia Department of Orthopedic Surgery.
Our mechanistic study is helping us to better understand how pairing brain and spinal cord stimulation can be combined. We are planning the translation to children using non-invasive techniques.
— Dr. Jason Carmel
Previous work by Dr. Carmel and researchers from the Movement Recovery Laboratory that was conducted in animal models provided the basis for this most recent study in humans. In the animal model study published in Brain, paired stimulation of brain and spinal cord was delivered to rats with injury to the cervical spinal cord. Rats that underwent electrical stimulation showed improved forepaw function when manipulating pieces of food and had stronger muscle responses to electrical stimulation, as well as near normalization of reflexes. These changes were not seen in rats randomized to receive sham stimulation. “If you’re a rat with a spinal cord injury, I can definitely help you,” quips Dr. Carmel.
Ultimately, these discoveries are setting the groundwork for the future of CP treatment. Currently, Dr. Carmel is the site Principal Investigator for NewYork-Presbyterian/Columbia in a multisite study examining spinal cord associative plasticity among patients 18 to 80 years. Patients who receive care at the Weinberg Family CP Center have access to novel trials not readily available elsewhere.
Transitional Program
Because CP is often not recognized until a child is 18 months or older, the multidisciplinary team works to repair injury that has occurred to the developing brain before, during or soon after birth, as well as provide lifelong, comprehensive care.
As the only dedicated transitional care program on the East Coast and one of just several in the nation, the Center is renowned for bridging care from pediatrics to adulthood and beyond. “There are only a handful of centers that are setup to do lifespan work,” says Dr. Carmel.
The multidisciplinary care provided by the team includes a lot of therapy-based interventions such as occupational therapy, physical therapy, speech, and interventions for swallowing difficulties. “We provide medical management to allow brain to heal and then manage secondary complications like orthopedic complications,” says Dr. Carmel.
Early Detection, Better Outcomes
The Weinberg Family CP Center seeks to provide lifelong care and early detection is one key aspect of this care. The Center has even partnered with the Division of Neonatology and Perinatology to lower the age of diagnosis of CP. “If we can detect CP early, then we can intervene early,” says Dr. Carmel.
Dr. Carmel’s team used to only perform genetic testing if an infant had risk factors such as prematurity or a brain bleed, but their protocol has changed based off of from results from a recent study published in Developmental Medicine and Child Neurology. “We found a high prevalence of genetic variants in kids who had risk factors for CP like prematurity or brain bleeds—either the gene is causing poor development of the nervous system leading to CP or the gene confers susceptibility to bleeds or prematurity,” hypothesizes Dr. Carmel.
By combining multidisciplinary and lifespan care with scientific innovation, the Weinberg Family CP Center is applying the best of today’s therapy while expanding treatment options for the future.