When faced with an infant diagnosed with biliary atresia, pediatric surgeons immediately invoke the legacy of Professor Morio Kasai, a Japanese pediatric surgeon who, in 1955, performed a successful hepatic portoenterostomy on a 72-day-old infant diagnosed with biliary atresia. Dr. Kasai had made significant contributions to developing that technique, which now bears his name. The Kasai procedure revolutionized therapeutic advancements in biliary atresia, providing a treatment option for a rare disorder that was considered an uncorrectable disease.
“The incredible influence of Dr. Kasai on the field continues to resonate to this day,” says Steven Stylianos, MD, Surgeon-in-Chief at NewYork-Presbyterian Morgan Stanley Children’s Hospital and Chief of the Division of Pediatric Surgery at Columbia. “My predecessor and mentor, the late Dr. Peter Altman, was intrigued by the disease and the operation. He and his colleagues traveled to Japan to learn the technique from Dr. Kasai, then championed the operation in the United States.”

Steven Stylianos, MD
R. Peter Altman, MD
Integrating Specialties for Continuity of Care
NewYork-Presbyterian Morgan Stanley Children’s Hospital is one of a few centers in the nation with the depth of clinical expertise to care for infants with biliary atresia. “From their presentation, babies with biliary atresia begin a continuum of care by our team of specialists in hepatology, interventional radiology, pathology, pediatric surgery, and pediatric liver transplantation,” explains Dr. Stylianos. “This multidisciplinary approach is the reason for our favorable outcomes. The care includes a collaboration among individuals evaluating patients, conducting surgeries, and analyzing outcomes. This is the type of team you need to go forward with such complex cases. Patients’ outcomes depend on incredible diagnosticians and hepatologists who know that the clock is ticking for these infants, and the great transplant surgeons ready to rescue these babies and send them on their way to a wonderful life.”
Dr. Stylianos’ role comes in at about the midpoint of this continuum when the diagnosis has been confirmed and the Kasai procedure is indicated. “It is an operation that, done skillfully and at the right time in the baby's life, can lead to an interruption in the progression of the disease,” says Dr. Stylianos. “I know that when I go to the operating room with a baby with biliary atresia, I am probably not going to be curative. But I can give that baby several, if not many years, of a healthy life prior to ultimate liver failure requiring transplantation.”
Timing is Everything
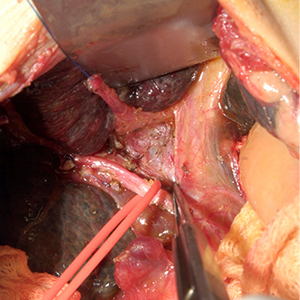
Kasai procedure (Courtesy of Dr. Steven Stylianos)
Biliary atresia is a complex, progressive disease with several phenotypes and numerous factors – still to be elucidated – involved in its pathogenesis. In a developmentally susceptible liver, those factors can progress into an activated immune response and significant inflammation. This inflammation ultimately causes tissue damage that results in fibrosis progression and eventually cirrhosis and liver failure. In fact, biliary atresia is currently the leading indication for pediatric liver transplantation in children.
With the harbinger of disease progression foremost in mind, Dr. Stylianos and his colleagues emphasize that biliary atresia is a time-sensitive diagnosis. “The research is unified on this issue. If the Kasai operation is performed before 60 to 70 days of life, there is a significant impact on favorable outcomes,” says Dr. Stylianos. “By expeditiously selecting patients for the Kasai procedure, our team can successfully delay the need for transplant for years and sometimes decades! As a result, the child won’t have to be on immunosuppressants or deal with the complications of liver failure from such an early age. That is a huge benefit for families.”
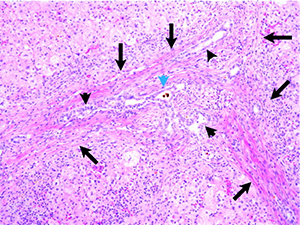
Pre-operative liver biopsy shows expansion of portal tracts with fibrosis, biliary ductular proliferation, and cholestatic plugs. (Courtesy of Dr. Steven Stylianos)
A liver biopsy is currently used to determine the signature signs of biliary atresia, such as ductular proliferation or bile plugging. Sheryl Tulin-Silver, MD, Director of Pediatric Interventional Radiology at NewYork-Presbyterian Morgan Stanley Children’s Hospital, has enhanced liver biopsy findings with a preoperative percutaneous cholangiogram imaging study, providing surgeons with a detailed roadmap before they perform the Kasai procedure. “Dr. Tulin-Silver’s approach represents a significant advancement in diagnosis and one that is now part of the overall workup of our patients, helping us to avoid unnecessary surgery,” says Dr. Stylianos. More recently, the team has begun exploring biomarkers to differentiate biliary atresia from other causes of cholestasis and may prove valuable in expediting a diagnosis.
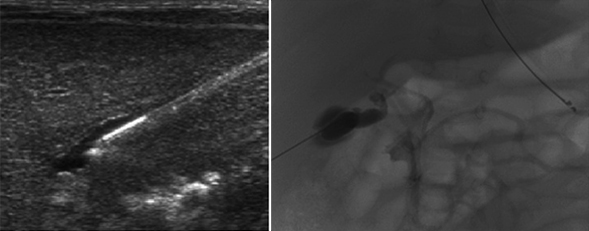
Percutaneous cholangiogram (Courtesy of Dr. Steven Stylianos)
“Anything that shortens the time from presentation to surgery is of value to patients with biliary atresia,” emphasizes Dr. Stylianos. “Those babies who clear their jaundice, and at least half should be expected to, and when the operation is done in the right interval of time, should have long-term success.”
Outcome Influencers
In sentinel research by Dr. Altman published more than 20 years ago that chronicled his 25-year experience with the Kasai procedure, he concluded that the risk of the Kasai procedure failure is related to age at the time of the surgery, as well as other factors, including bile ductal anatomy, liver and portal plate histology, and the biliary conduit.
“Neither gender, race, histology, associated anomalies, or the type of conduit constructed, were independent risk factors,” says Dr. Stylianos. “If jaundice was completely cleared after undergoing Kasai, the median survival without transplant was up to 15 years of age. The outcomes and the reasons behind them identified by Dr. Altman hold true to this day. Recent analysis shows that an estimated 60 percent of children operated on for this condition at NewYork-Presbyterian Morgan Stanley Children’s Hospital were jaundice-free two years after surgery, which is about 10-15 percent better than most reports. We will keep seeking early diagnostic and therapeutic strategies to refine the Kasai procedure and improve the outcome of infants with this challenging disease.”



